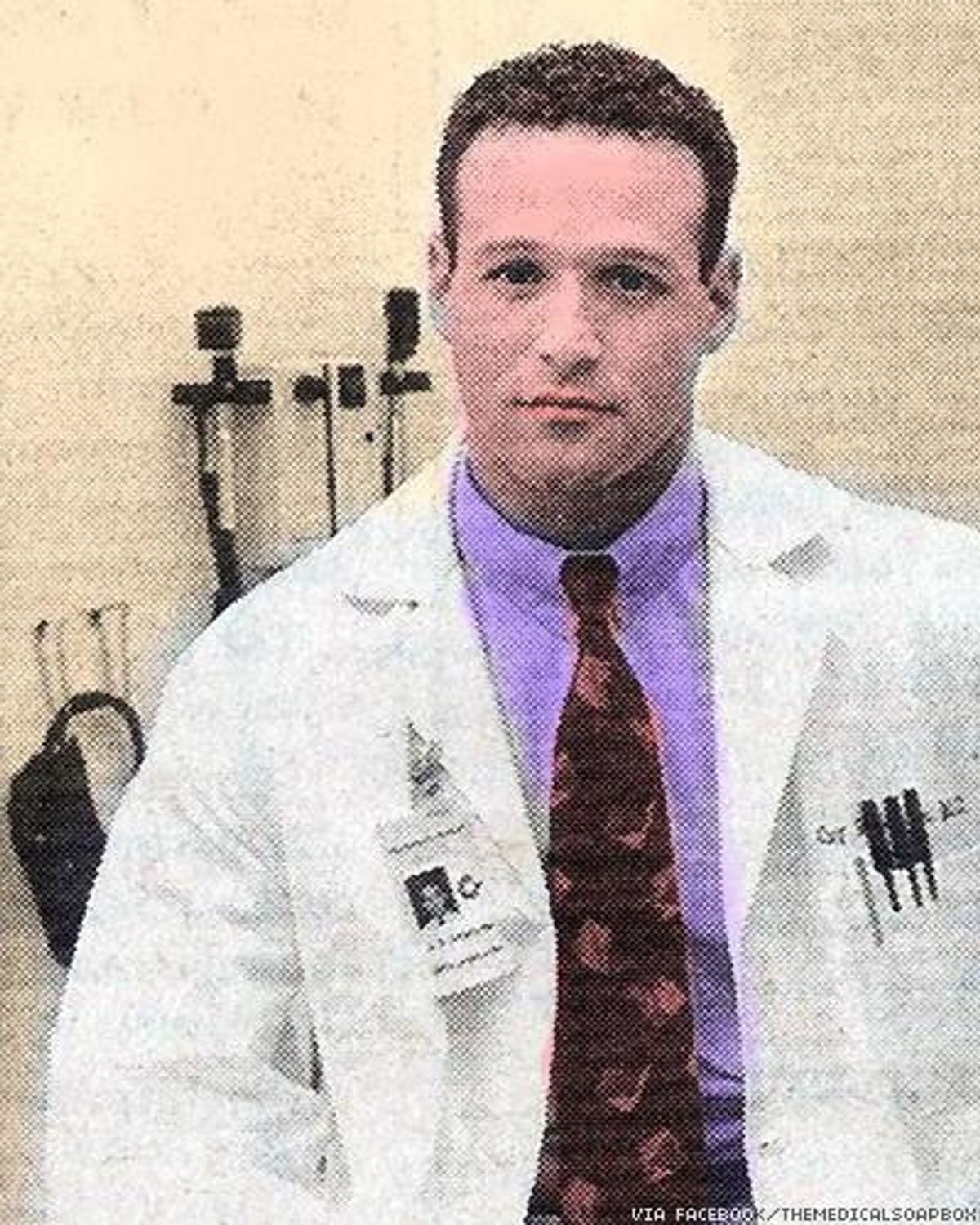
The Advocate: Tell us in your own words why you support PrEP for use by gay men. Did the Centers for Disease Control and Prevention recommendations affect you? Were you prescribing it before then?
Gary Cohan, MD: Yes and yes. I was prescribing it before then, for my very high-risk patients. But after the CDC and the World Health Organization recommendations came out earlier this year, it just lent credence to what we were doing and allowed us to expand it to the more general sexually active population. To answer your first question, though, what's been happening is Truvada for PrEP has been approved since 2012, and if you look at the number of HIV infections in the United States, we've had the same exact number -- 50,000 new HIV infections every year since the '90s. So we are completely fulfilling Albert Einstein's definition of insanity, which is we're doing the same thing over and over again but expecting different results by saying, "Preach condoms, preach condoms, that's it." Well, along comes a medication that has data -- and this is with an asterisk for a moment -- that has data that shows that this could drastically reduce new HIV infections and protect people, yet you have some people still clinging to antiquated ideas about safer sex. This is a revolution! This should be above the fold in The New York Times and on the cover of Time magazine. A pill to prevent HIV infection?
There's criticism of Truvada as PrEP.
All the criticisms of it make no sense whatsoever. And if you want to go through each one by one, we can, but the point being, if all the guys that died from HIV that I took care of - in the '80s and '90s - if they were all magically able to come back and I said, "Hey, guys, you know there's a pill to prevent HIV?" would they feel like they would want to take it? Of course they would. Some people say that somehow dishonors their memories and we should just heed the advice of our own history and preach condoms only.
But that's a mistake?
What the new safer sex is -- and that's kind of what we're really dealing with -- I mean, they've even come up with a name for it. I think it's a little cumbersome. It's called "high-impact combination prevention strategy," where we're counseling the patients about safer sex. We are talking about barrier condom use; we're talking about drug use, which is often in the context in which people get infected; we are talking about reducing the number of sexual partners people have; and we're also talking about pre-exposure prophylaxis with Truvada. Meanwhile, there's been more statistics: The rate of HIV infections from 2002 to 2012 dropped by about 33 percent in minorities and women, while at the same time it went up 133 percent in gay men. [Sighs] And that's just so disappointing. Because that's the group we'd hoped would have learned the lessons of history.
We're a generation up from the first generation that was impacted. There are one pill, once-a-day treatments. You don't any longer see the skinny purple spotted guys limping around with canes to give you a visual reminder of what you don't want to get. And just the general lack of perception of mortal threat has coincided, in sort of a perfect storm, with a generation that didn't experience it. Then the online hook-up apps have made frequent and multiple sexual partners possible at the same time. As horrifying as it may sound to people who, like myself, witnessed the entire AIDS epidemic from the very beginning, bareback sex -- condomless sex -- has come back in vogue. Even in pornography, that's being depicted on multiple sites. We would've protested and picketed those sites or those studios in the past, and now it's become kind of de rigueur. It's become what people want to see; they don't want to see condoms because it isn't considered sexy. And condoms were never anybody's first choice. I mean, they reduce spontaneity, they reduce sensation, they just are something that gets in the way of the moment. And they were never consistently used, which is why we have all of those infections.
So no matter how much we keep preaching condoms, they are just not going to [resolve this]. Even if barebacking wasn't as popular as it is now, they are just not going to get used all the time.
And you know sex is sort of a time when people let their hair down and let their inhibitions down and, you know, certain body parts get poked into other body parts. And body parts may be covered or uncovered during certain points. You're not quite sure: Was that safe? Was that unsafe? Even if somebody is committed to condoms, I know lots of people who come to me with questions, "Hey, this happened -- we were about to put the condom on and he was inside me for just a second." And I will say, look, I don't know. There can be pre-come or pre-ejaculated fluid at the end of the penis once it's erect, so there's always the possibility, so we always have to weigh the risks and benefits of post-exposure prophylaxis [PEP], which is a bit dicey. What I think PrEP represents for the responsible crowd is, it fills in all those tiny little gaps. I like to fix up houses, so it's like spackle. It fills in all the little holes where you might have had a very minor exposure or potential exposure and it's going to protect you.
A friend said to me, "You cannot imagine, as a gay man, what it's like for the first time in my life to not worry I'm going to get HIV, or that I'm not going to give HIV to somebody else."
Those words are the exact feedback I get. They come in almost in tears of joy, saying "I feel like a different person." But I'm not letting up my guard. Researchers studied whether people who use Truvada have unsafe sex and the answer is, it doesn't encourage sex without condoms. The iPrEx study that was published on July 22 of this year saw no increase in risky behaviors. The guys who are doing this want to have as safe sex as possible. They would like to stay negative.
So take me back to what you tell your patients about PrEP, about the side effects, the requirements. Before anyone begins, what did you tell them?
I actually create a script that we read together. It's one piece of paper, double-sided, and we go through it literally bullet point by bullet point. So I tell them that there's new evidence suggesting that people who take PrEP, which is Truvada, that they dramatically reduce the risk of acquiring HIV and that both the CDC and World Health Organization officially recommend it for high risk. That it's taken every day without missing doses. That it's not effective immediately, that it can take one week to reach effective levels in rectal tissue and three weeks to reach maximal levels in the bloodstream and vaginal tissue. So again, you can't just take it today and think that you are fully protected tomorrow. That you still have to use other HIV prevention methods and condoms and reduce your number of partners and not be impaired by drugs during sexual relations. That you get regular checkups at about three-month intervals and we check you for various STDs, we check kidney function and anything else that's appropriate -- hepatitis serologies. That it doesn't protect you from any other STDs -- syphilis, gonorrhea, chlamydia, HPV, hepatitis. That they must be vaccinated for hepatitis A and B and I encourage them to get vaccinated with the Gardasil shot for HPV before starting. That it may not be 100 percent effective, that we're waiting for this but that the data is looking in the direction of being so good and there's no time to waste. When you're dealing with a lifelong, potentially fatal infection, is it right to withhold it until the last drop of data is in, if it's looking as good as it is? And the answer is no, that's not appropriate and that's not how we've operated the whole HIV epidemic. We had HIV trials when AZT, ddI, ddC -- go on down the list -- before we had the final data. So this is utterly consistent with how we've managed the epidemic. We basically, not really went out on a limb, but we basically looked at data and if it was compelling enough, we explained to our patients carefully the risks and benefits and treated them like adults, and then said the decision is ultimately yours but we would like to be able to either treat you or help prevent an infection. That's served us very, very well.
If a person who is going on this drug doesn't have a relationship with their doctor in which they feel comfortable talking about all of this, would you recommend that they try to find somebody different?
They should. You know there's two parts to that. If they have access to the Web, they should probably go to PrEPFacts.org because that's the best patient friendly site out there, and if there is an HIV-specializing provider -- hopefully somebody who's accredited by the American Academy of HIV Medicine -- then they should look that up. They can go to their website and put in their zip code and try to find a doctor in the area. So the answer is yes, I would feel more comfortable with somebody who knows what they are doing.
Now I also tell them about the potential side effects. You have to remember that Truvada was approved in 2004, so I've had people on this for over a decade and the ingredients in Truvada were approved even before that, because it's a 2-in-1 drug. And I've almost never seen any side effects from it. They mention headaches and nausea and diarrhea and that kind of stuff and I almost never see it. And even if they do get mild side effects, they go away within a couple of weeks. Long-term, and this is in HIV-positive people, we have seen some kidney dysfunction and some loss of bone mass, but again, if somebody comes in and they've got normal kidney function at the baseline, the likelihood that we're going to get into trouble with Truvada is, I think, pretty small. And the studies have never shown any major toxicity; but you do have to monitor for that. And so that's part of testing on follow-up. But again, those are usually long-term patients on HIV drugs.
And remember, HIV beats the heck out of the kidneys too. And it's age also; our kidney functions decline about 1 percent a year in all of us human beings, positive or negative. In HIV-positive people, HIV beats on the kidneys, and then Truvada can aggravate that. So a long-term patient on Truvada as part of their HIV regimen may be at much higher risk than somebody who was using it for PrEP. So I also tell them what is the effectiveness based on the data or, you know, the maximal effectiveness. So with daily use, zero missed doses, it's up to 99 percent effective. Four days a week, they say up to 96 percent; and something more recent said four days a week may be closer to 99 percent. But again, you know, 99 percent for daily, 96 percent for four days a week, and up to 70 percent for two days a week, and that's an interesting statistic because that's the same efficacy as condoms.
Wow, that seems like a game-changer.
Now again, I might say over and over again, "Condoms have to be a part of it." But we all know -- it's sort of the secret I dare not speak its name -- but you know, condom use is just not happening the way it used to. Maybe it was never happening the way we thought it was. We have to deal with things as they are, not as we'd wish them to be, and do our best to protect the people when we're charged with their care.
So I go over that. I determine: Are you a person who's ready for PrEP? So let's say they're in a monogamous relationship, they're both HIV-negative. Well, it kind of depends. I'll ask them, and some patients have been together a very long time and they say we really don't venture out anymore and so it's really unnecessary, and they trust each other. OK, I'll have to accept that at face value. If you have people who are in an open relationship, then they should consider PrEP strongly. There's always a risk that somebody has a dalliance and doesn't tell the other partner, and that's their own communication issue and they need to learn to communicate that. In my own relationships -- knowing that people are fallible -- I've always had the rule that anything can be forgiven, but if one of us has a dalliance or sex outside the relationship, then you've got to tell the other partner to protect them. And that's always been the case in my relationships and has not failed me. There's shame involved and there is guilt involved and so it may not be perfect, but I think that's the best we can do.
I don't think that PrEP is appropriate for everybody. I have some people who really are not sexually active; well, they don't need it. I have people who are truly in monogamous relationships, and they don't need it. I ask them all, you know, I get very personal with them and ask them about their relationship and sometimes actually I bring both partners in at the same time to kick it around with me.
When you're talking to your patients about this, are you seeing a common thread in terms of what they're concerned about?
First thing they ask is, "Does insurance cover it?" [Laughs] And to date? Yes, insurance does cover it. Gilead has a pretty robust patient assistance program, so I haven't had anybody who hasn't been able to get it, is the bottom line.
The other things they ask me about is toxicity. They ask me, "Well, what about this stuff about how it doesn't really work?" And I go through the data there and explain how the data has been misconstrued of misrepresented, and I also say that we're not finished with all of our studies; that they are being pioneers, that there could still be some risk, but we think that this reduces risk and the uptake has been almost 100 percent. After the conversation, I've never had anybody who said -- because I make them sign off on this sort of information/consent form that I've created -- and I've never had anybody that's not consented. And this is a pretty detailed consent form. I even put in if you get infected what does that feel like? A primary HIV infection? So I put down all the mono-like symptoms that are there. All the points I've discussed with you are condensed into this thing that we go over point by point, and I don't skip over anything. I mean, we literally go through everything because, again, if they are the pioneers here, I always want to err on the side of caution, where we have some question marks.
So a patient would be on a PrEP schedule? He would get a reminder every three months, and then what would you be testing for at that three-month point?
Well, let's talk about one really important thing. They must test HIV-negative with the PCR test before we start. Because if I'd put them on Truvada and they've just acquired HIV and they don't know it, I'm going to make them resistant to Truvada, because it's not a fully effective HIV treatment. It's good for prevention, but you need three drugs [for treatment] and that's only two. So they have to do that beforehand with some other kidney testing and hepatitis testing, etc., in terms of the testing, you know, at various intervals. I give them an STD check -- which is HIV, gonorrhea, syphilis, chlamydia -- I do a hepatitis panel, I check their kidney function. I typically check their liver function as well. At the three-month visit I also ask them about side effects. I don't give them more than a 90-day prescription; they get 90 days but no more. So that encourages them to come in. I estimate it out: Are you taking it every day? Are you having trouble? I give them some adherence counseling. I ask them about risk reduction behaviors, about drugs and sexual partners. And if they have any new questions or anything new comes up, that's what we look at.
Should patients be thinking about Truvada or PrEP for a lifetime?
This was the first drug studied that we currently have. The data is, to all of us, surprisingly good. And we're going to get better. Just like the HIV epidemic, we started with AZT, which was a start, but not so good. And then we ended up with combination therapies with three-time-a-day protease inhibitors that cause lipodystrophy and kidney stones and all kinds of stuff, and then we got better and now we're down to a bunch of one-to-once-a-day combination pills that don't seem to cause any side effects. So it's going to evolve just like that. But this is out of the gate.
Again, this is a drug that has been around for so long. There's a misconception that this is somehow a new drug. It isn't. It's an old drug. We're just repurposing it. So in terms of being for or against, it doesn't make any sense to be against it.
Lots of people have compared this to the early days of the birth control pill with the slut-shaming and other things that went on, and now there's sort of not any real issue about the birth control pill -- other than the fights about insurance coverage. Anything that has to do with sex, it can, for some people -- doctors, patients, government bureaucracies, insurance companies -- they can get a little weird about it.