Since the first National Women and Girls HIV/AIDS Awareness Day in 2006, we've witnessed noteworthy milestones domestically in the fight against HIV/AIDS for women including: the availability of new highly effective HIV treatment and prevention options, new health plans offering HIV screening with no cost-sharing under the Affordable Care Act, the first comprehensive National HIV/AIDS Strategy for the U.S., and the formation of a federal working group to coordinate efforts specifically on the intersections of violence against women, HIV/AIDS, and gender-related disparities. We can be proud of this progress, with promising data showing that HIV diagnoses among women in the U.S. have declined by an unprecedented 40 percent between 2005 and 2014.
But, even as we celebrate these and other milestones, gender and racial inequality continue to rage in the background; I am reminded that today as a woman living in Washington, D.C., I have a 1 in 70 chance of being HIV positive; if I'm black, my chance jumps to 1 in 38. I have a 1 in 3 chance of being abused by an intimate partner, a 1 in 8 chance of not having health insurance, and a 1 in 2 chance of having an unintended pregnancy before I turn 45. My health needs, like that of all women, are complex and related -- influenced by my race, geography and behaviors.
In this decade we have seen persistent racial disparities in HIV, continuous battles to restrict the sexual health and reproductive rights of U.S. women, and the devastating effects of gender-based violence, which continues to affect 55 percent of HIV-positive women -- double the national rate.
HIV/AIDS is a disease of opportunity. One only has to follow the trail of pre-existing health and social disparities to find where new infections are escalating. Black women are 20 times more likely to be diagnosed with HIV than white women, and represented 64 percent of all women living with HIV in 2011. Rising racial disparities in HIV remind us that despite advances in treatment and prevention, women -- and particularly women of color -- will not benefit equally if the long list of existing social inequalities is not addressed.
HIV/AIDS is not a disease in isolation. HIV among women is inextricably tied to other sexual, reproductive, physical, and mental health needs, as well as fertility desires and partner dynamics. Family planning sites are a critical provider of women's medical care, with 60 percent of women reporting that a family planning clinic is their usual source of care, and 41 percent reporting that it is their only source of care. Restrictions on women's access to sexual healthcare and rights, including the closure of family planning clinics, send ripples through our nation, negatively impacting not only women's reproductive health but HIV care and wider preventative healthcare access.
Intimate partner violence continues to affect women and girls at epidemic proportions, with 35 percent of women in the U.S experiencing rape, physical violence, or stalking in their lifetime. Violence can increase a woman's risk for HIV by exposing her to forced sex, limiting her power to negotiate safer sex practices, and increasing future sexual risk-taking behaviors. HIV/AIDS may be just one of many competing health priorities for women, who may be struggling to stay safe from violence, care for children or aging parents, or manage other chronic health issues.
Social drivers of HIV infection, such as barriers to healthcare access and violence, are even more severe for transgender women, who despite having some of the country's highest infection rates, are routinely left out of programming and research. Transgender women face high rates of discrimination and social stigma in healthcare, education, employment and housing -- negatively impacting their physical, mental and economic wellbeing. Although limited, non-probability studies have shown about a third of transgender women in the U.S. are estimated to be living with HIV; however, the generalizability of these data are largely unknown and desperately requires greater research attention.
During this National Women and Girls HIV/AIDS Awareness Day, I am reminded of the progress we've made as a country to combat HIV among women and girls, including seeing new HIV diagnoses among women decline faster than almost any other U.S group, outside of people who inject drugs. However, we must address the contextual issues that put women at risk for HIV in the first place. Battles over women's health access are happening now, as the Supreme Court debates the constitutionality of a 2013 Texas law that could lead to the closure of all but eight of the state's clinics providing abortions and other critical preventative health care for women. Unfortunately, this is just one of 231 new restrictions that have been imposed on family planning clinics by 22 states since 2010.
If we intend to make further gains in the fight against HIV, and indeed to eliminate HIV in women and girls, it is not enough to fight the virus. We have to fight to make women's health a larger policy priority -- ensuring that we respond comprehensively to women's sexual and reproductive health and rights.
JENNIFER SHERWOOD is a Policy Associate for amfAR, The Foundation for AIDS Research.








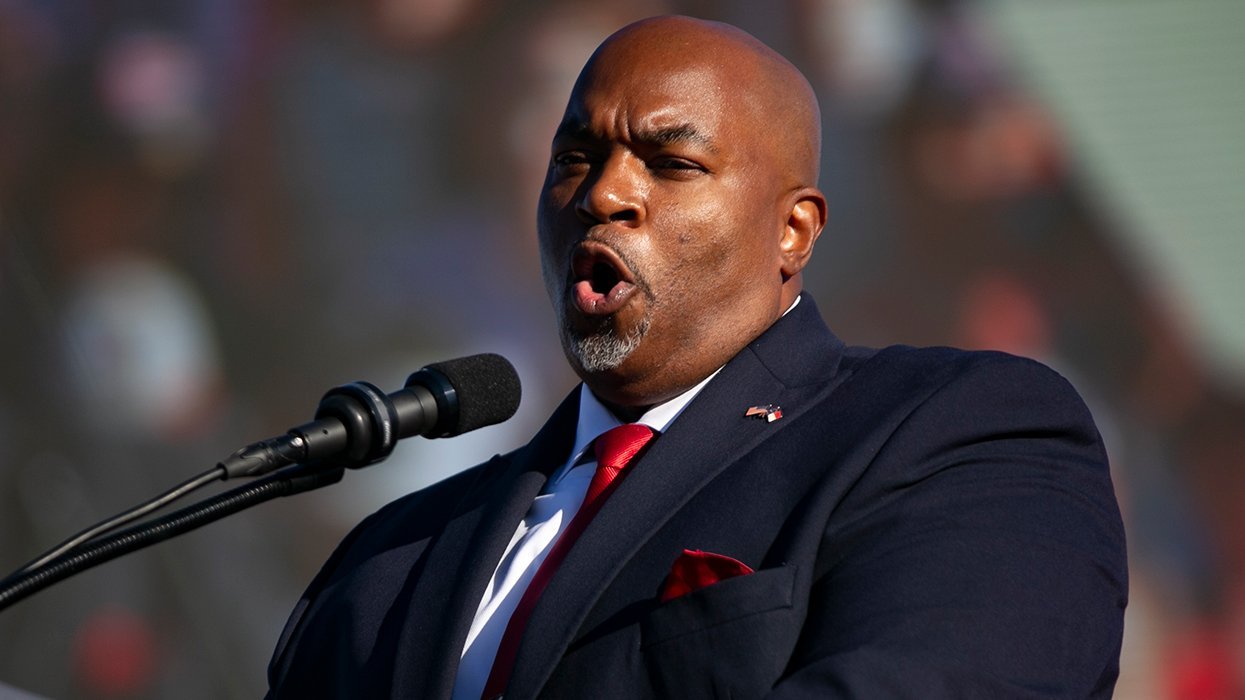








































































Viral post saying Republicans 'have two daddies now' has MAGA hot and bothered