On March 18, Colorado joined California, Oregon, and the District of Columbia in expressly prohibiting discrimination in health insurance due to sexual orientation or gender identity.
In a bulletin published by the Department of Regulatory Agencies' Division of Insurance, the agency clarified that any insurance provider offering health care within Colorado may not deny, cancel, limit, refuse to issue or renew, or charge more for health insurance to a client based on the insured's sexual orientation or gender identity.
Statewide LGBT equality organization One Colorado lauded the bulletin as "an important victory for the health of all Coloradans," and summarized the bulletin's key points. According to One Colorado:
"Health insurance plans sold in Colorado can no longer:
1) impose higher rates or charge more because of an applicant's sexual orientation;
2) use an individual's sexual orientation as a pre-existing condition for the purpose of limiting or denying coverage; or
3) deny, exclude or limit coverage for medically necessary services as determined by an individual's medical provider, if the same item or service would be provided -- based on current standards of care -- to another individual without regard to their sexual orientation."
While the bulletin is not legally binding, it is intended "to provide guidance about the antidiscrimination provisions of state law ... based on sexual orientation," which the Colorado Antidiscrimination Act defines as "a person's orientation toward heterosexuality, homosexuality, bisexuality, or transgender status or another person's perception thereof."








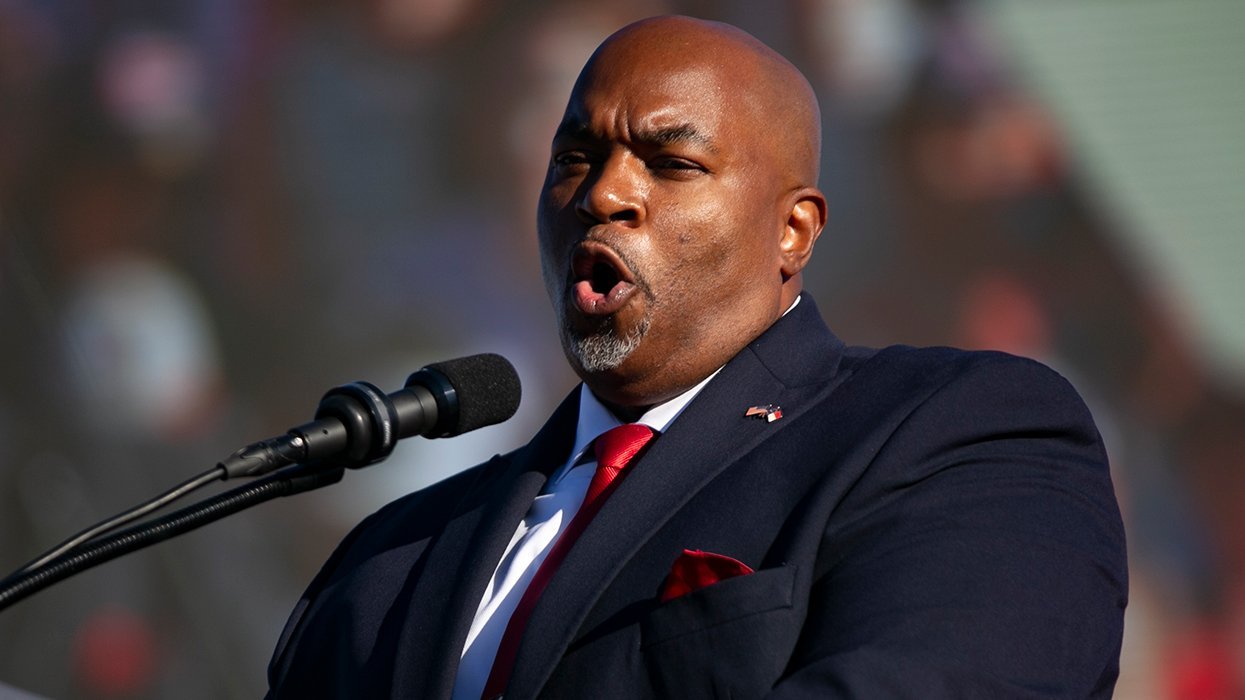









































































Viral post saying Republicans 'have two daddies now' has MAGA hot and bothered