In order to slow the spread of HIV, certain people who do not have the virus but are at risk should take medication to prevent becoming infected. That's the recommendation of the Centers for Disease Control and Prevention, and just recently, the World Health Organization.
The preventive treatment is known as PrEP, for pre-exposure prophylaxis, and the only drug approved for it so far is Truvada, which is also used to treat those already infected, and is a combination of two medications.
Eric McCulley made the decision to start PrEP. He's 40, he's gay, and he's HIV-negative. Outside an Atlanta coffee shop, he pulls out a small plastic bag with a few blue pills.
"They're a decent size, actually," he says. "Some people might call them a horse pill."
After hearing about the use of Truvada for prevention and doing extensive research on his own, McCulley consulted with his primary care doctor.
"He was very supportive about it. He encouraged me to do it," he says. "He gave me a lot of stuff to read, gave me a lot of stuff to think about, and told me I was a good candidate for it. So off we went."
A few months into his Truvada regimen, McCulley says the only change has been is in his attitude.
"I have what I was looking for. I have peace of mind. I feel like I've taken responsibility for my health," he says.
But some PrEP users worry that not all doctors are up to speed. Although Truvada has been on the market for a decade, its use for prevention was approved just two years ago by the Food and Drug Administration.
Dylan West, a 25-year-old gay Atlantan who works in international aid, has found out firsthand that not every doctor is as familiar with PrEP as McCulley's.
Some gastro-intestinal issues recently landed West in the emergency department. He'd started PrEP after beginning a relationship with someone who's HIV-positive. One of the doctors in the emergency room noticed that West listed Truvada as a medication he regularly takes.
"She immediately, without asking any questions, just said 'Well, we should probably test for gonorrhea, syphilis, HIV/AIDS -- the list,'" he says.
West feels that physician made a "rash assumption" about his sexual practices because he was on Truvada. West knew stigma was something he might face.
"The assumption being, you're on Truvada, so you probably run around having sex with whoever you can," he explains.
Some health advocates and LGBT activists have gone so far as to label those on PrEP as "Truvada whores."
Melanie Thompson, MD, says she's heard that before. She's the principal investigator of the AIDS Consortium of Atlanta and has long worked in HIV research. She has encountered reluctance from some to prescribe PrEP because of lack of knowledge about it.
"This is an interesting thing to me," she says, "because doctors who say, 'I don't want to prescribe PrEP to somebody who might be at risk for HIV because they might not use condoms' -- you know, it's an approach we wouldn't take in other areas of medicine."
Thompson says no doctor would refuse to prescribe cholesterol-lowering statins to patients because they're overweight. Somehow, the conversation around PrEP is different.
"So I think it's a very interesting moralistic attitude that soon will be outdated. But I do think that this is a barrier for some patients," Thompson says. "They feel stigmatized. And honestly, health care providers need to step up their game and do better than that."
A CDC spokeswoman says lack of awareness and knowledge among health careproviders is one of the primary challenges to PrEP's success.
But both Thompson and CDC officials hope the newly issued guidelines on use of PrEP will help overcome any barriers.
This article was provided by Kaiser Health News, which is an editorially independent program of the Henry J. Kaiser Family Foundation, a nonprofit, nonpartisan health policy research and communications organization not affiliated with Kaiser Permanente.








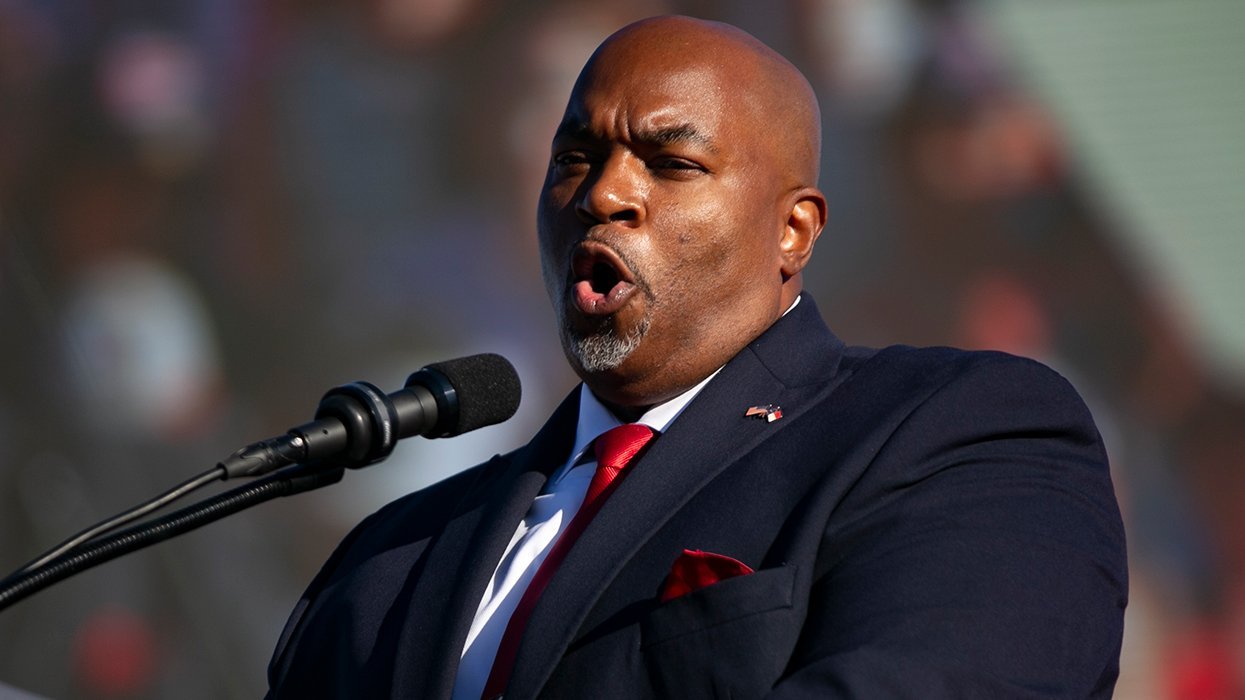








































































Viral post saying Republicans 'have two daddies now' has MAGA hot and bothered