CONTACTAbout UsCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Equal Entertainment LLC.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
We need your help
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
These days, it's common for HIVers to receive lab tests to predict how their particular strain of virus will react to various medications to determine potential drug resistance, allergic reactions, and so on. But imagine if a genetic screen could instruct a medical team how best to train your immune system to fight the virus on its own, possibly without the need for daily antiretrovirals.
The study of such gene therapies, currently in its infancy, has the theoretical potential to revolutionize HIV care in the next five to 15 years-at least in countries that can afford what may be a hefty expense. At minimum, gene therapy could prove a hearty partner to highly active antiretroviral therapy, perhaps better suppressing viral loads, lessening pill burdens, or allowing for structured treatment interruptions. Standing in the way of such progress, though, are the vast unknowns of the new field.
"We need to be better than nature," says Nobel laureate David Baltimore, MD, a professor of biology at the California Institute of Technology. Baltimore is attempting to manufacture synthetic antibodies that can fight HIV in a way that ordinary human antibodies have failed to.
While the pipeline for new anti-HIV meds has hit a dry patch -- no major new drug is expected to be approved in the next couple of years -- a handful of small biotech companies and intrepid academics, such as Baltimore, are stirring a genetic wave for the future.
"In light of all the issues around antiretroviral therapy -- with costs, with unknown side effects, with the difficulties of adherence, all those things -- an approach like gene therapy is really exciting," says Matt Sharp, director of treatment and prevention advocacy at Project Inform in San Francisco. "The field is clearly moving forward, albeit slowly."
"Anything that could get people off antiretrovirals, even just for an extended period, could be a huge thing," seconds Richard Jefferys, a treatment advocate with Treatment Action Group.
The Obstacles
Current anti-HIV gene research largely involves variations on a similar theme. First, the scientists remove a collection of immune cells from an HIV-positive person's body, be they T cells or the stem cells that manufacture them. Second, they use what are called vectors to insert one or more new genes into those cells. These vectors are actually viruses themselves, and they have the capacity to cut and paste DNA strands to insert new genetic instructions. The modified cells are then put back into the patient. Finally, a waiting game follows as researchers see if the cells absorb well into the immune system, how long they last, and how successful they are at fighting HIV.
In an ideal setting, perhaps bordering on science fiction, the reprogrammed cells would permanently change the immune system. Scientists more realistically anticipate such a treatment would likely have to be repeated once or twice a year.
Like combination antiretroviral therapy, which uses different classes of medications to attack the virus at various stages of its life cycle, the best gene therapy will probably have multiple targets. John Zaia and John Rossi, researchers at City of Hope, a cancer research center in Southern California, are studying patients who are undergoing treatment for AIDS-related lymphoma. As with any bone marrow transplant treatment, a new immune system is infused into the patient after the other is wiped out by chemotherapy. Zaia and Rossi are attempting to manufacture a number of immune cells whose genetic codes have been rewritten in three different ways to better fight HIV and to include those cells with the transplant.
Like many others in his field of study, Zaia says the case reported in 2008 of the German man who was effectively cured of HIV after receiving a bone marrow transplant during treatment for leukemia proves the genetic method of attacking HIV can work. Replicating that one case, however, is not practical. There is a one-in-10-million chance of finding a donor who is both a match for any one bone marrow type and who has the particular genetic abnormality that is resistant to HIV infection, as was the case with this man. (Only 1% to 2% of humans have CD4 T cells that lack the CCR5 coreceptor, which most strands of HIV need to latch on to in order to enter a T cell. These people are thought to be naturally resistant to HIV infection.) The trick is finding a way to manufacture such resistance synthetically and then successfully transplanting the cells without the need for potentially lethal chemotherapy.
For example, Carl June, a cancer researcher at the University of Pennsylvania, is attempting both to create CD4 T cells that lack the CCR5 coreceptor and also to train CD8 T cells to recognize HIV more quickly and kill the virus more effectively.
Making Progress
Thus far, Ronald T. Mitsuyasu, MD, director of the University of California, Los Angeles, Center for Clinical AIDS Research and Education, has made the most progress with his research. He has manipulated the stem cells in his patients to produce T cells better equipped to inactivate HIV genes. He has since published the first randomized, double-blind study that proves it's possible to safely use genetic therapy to lower viral load and to raise T cells during a structured treatment interruption.
"This is a very new field with very little data available, and so I do not want to get patients' hopes up too high, since it will take a long time for this therapy to be an effective and feasible way to treat HIV on a routine basis," Mitsuyasu cautions, noting that his results were very modest.
Researchers and treatment advocates further caution that gene therapy comes with potential unknown risks.
"I think that for anybody who's thinking about participating in a trial," Jefferys says, "one thing to think about ahead of time is the fact that they're going to want to keep track of you for a long time and that there are potential risks that they might just not know about yet."
Outside of the scientific difficulties, the success of such new treatments largely depends on money. Currently, there isn't much of it to spend on research. The Bill and Melinda Gates Foundation, for example, which has spent more than half a billion dollars in the search for an HIV vaccine, has so far contributed a comparatively modest $14 million to this field of research, all in the form of a single grant to David Baltimore at Cal Tech.
On the back end of the financial problem is the issue of accessibility. The current method of taking cells out of the body and putting them back in is labor intensive and could cost tens of thousands of dollars per treatment. Researchers agree that they must discover a way to inject a gene therapy into HIVers that will find the immune cells and change their genetic makeup inside the body, not in the laboratory. This one-step process would greatly reduce the cost.
But even if such a single injection is itself still costly, genetic therapy could save money over time.
"If you're showing that you're going to improve people's quality of life and you're going to reduce their drug expenditures because they could have five years off day-to-day drug therapy," Jefferys says, "then you're looking at something that could really be financially practical."
From our Sponsors
Most Popular
Bizarre Epstein files reference to Trump, Putin, and oral sex with ‘Bubba’ draws scrutiny in Congress
November 14 2025 4:08 PM
True
Jeffrey Epstein’s brother says the ‘Bubba’ mentioned in Trump oral sex email is not Bill Clinton
November 16 2025 9:15 AM
True
Watch Now: Pride Today
Latest Stories
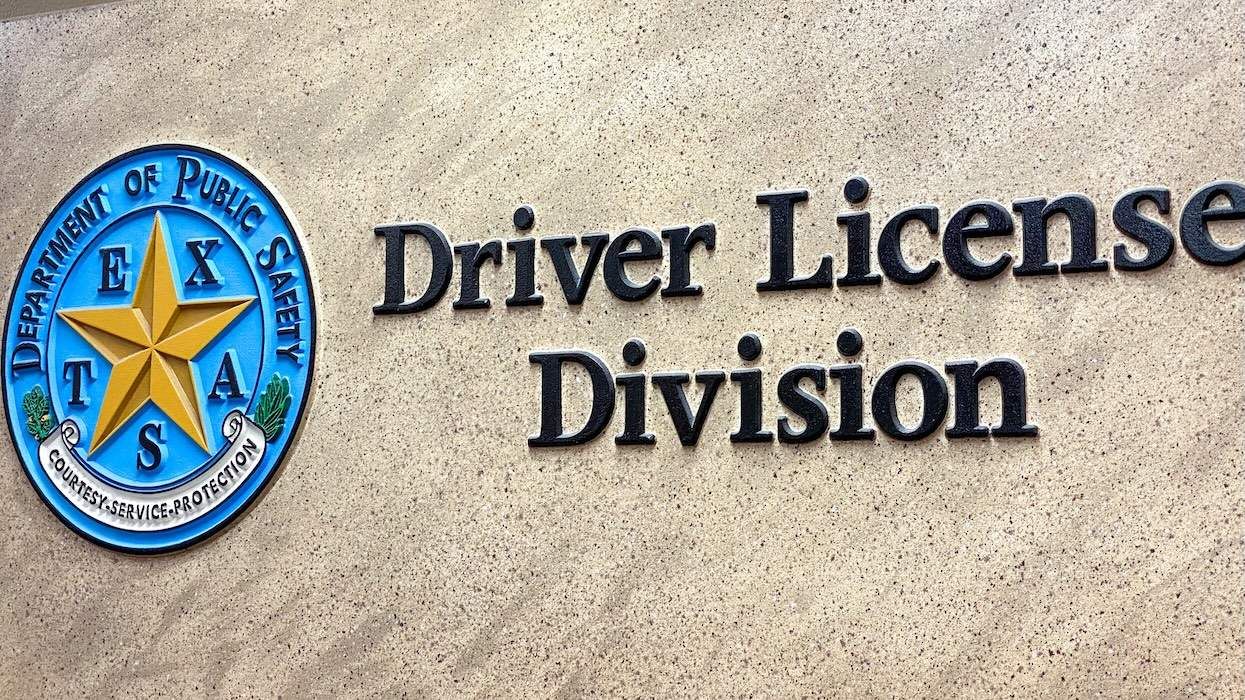
Is Texas using driver's license data to track transgender residents?
December 15 2025 6:46 PM
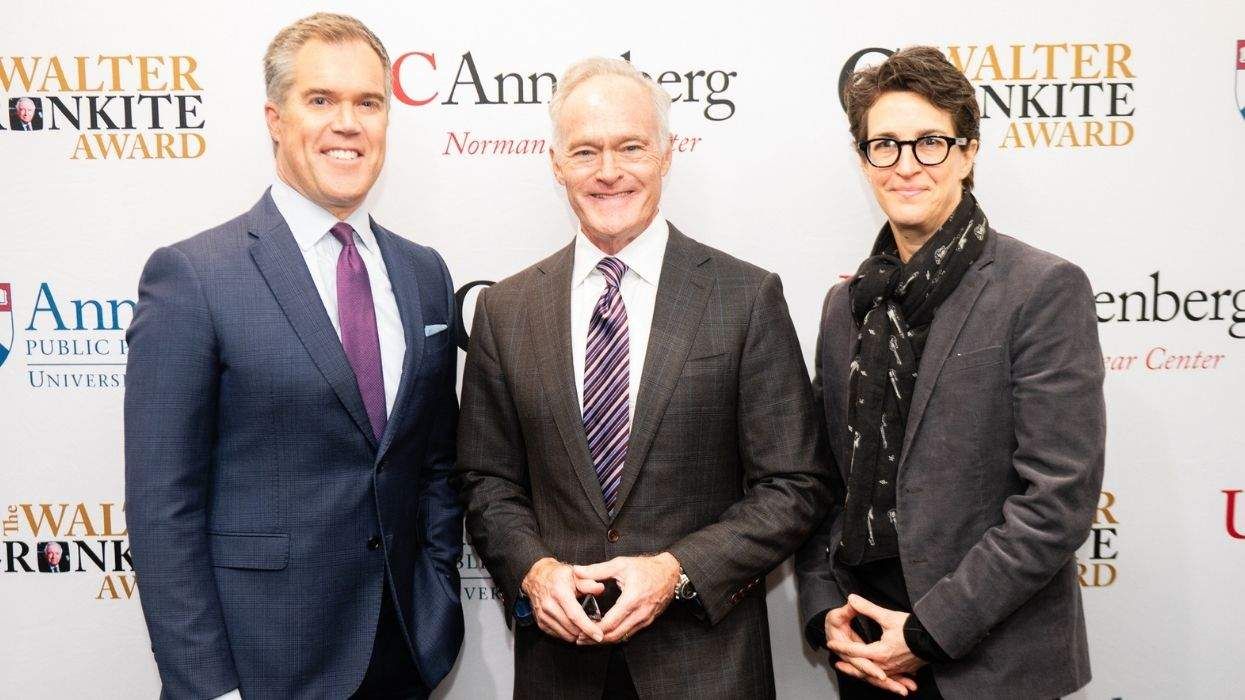
Rachel Maddow on standing up to government lies and her Walter Cronkite Award
December 15 2025 3:53 PM
Beloved gay 'General Hospital' star Anthony Geary dies at age 78
December 15 2025 2:07 PM
Rob Reiner deserves a place in queer TV history for Mike 'Meathead' Stivic in 'All in the Family'
December 15 2025 1:30 PM
Culver City elects first out gay mayor — and Elphaba helped celebrate
December 15 2025 1:08 PM
Texas city cancels 2026 Pride after local council rescinds LGBTQ+ protections
December 15 2025 12:55 PM
North Carolina county dissolves library board for refusing to toss book about a trans kid
December 15 2025 11:45 AM
Florida and Texas launch 'legal attack' in push to restrict abortion medication nationally
December 15 2025 11:18 AM
No, Crumbl is not Crumbl-ing, gay CEO Sawyer Hemsley says
December 15 2025 10:12 AM
11 times Donald Trump has randomly brought up his ‘transgender for everybody’ obsession
December 15 2025 9:22 AM
The story queer survivors aren't allowed to tell
December 15 2025 6:00 AM




























































Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes