CONTACTAbout UsCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Equal Entertainment LLC.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
We need your help
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
In the five years since he was infected with HIV, Larry Reigel has had a virtual systemic breakdown. Most recently hospitalized for epileptic attacks and severe neuropathy (nerve loss in extremities like hands and feet), he's been sluggish, had no sexual appetite, and feels dried out. He also suffers from diarrhea, hair loss, and chronic indigestion.
"It's all the effect of the AIDS medications," says Reigel, who lives in Philadelphia. But even unpleasant interactions are better than going without medicine. He adds, "My doctor said I went though the gamut of HIV meds, so I'm on my last reprieve."
Across the continent in San Francisco, Rob Rosen has been living with HIV for at least 24 years. Rosen is gay and a former drug user, and suffers from a double whammy of HIV and hepatitis C. Diagnosed in the 1980s, he was asymptomatic for years and only started taking meds in 2001. Since then, he's watched his T cells (the white blood cells that fight HIV, counted as a general indication of how sick a patient is) go down, although his viral load (the amount of the virus in a blood sample) remains low.
"I've been on the protease cocktail since 2001," he says. "I've begun a new regimen with Isentress, a new class of drugs, integrase inhibitors. It's an alternative to doing protease inhibitors, which have a huge gastrointestinal effect. This is no picnic for me."
These two men have two entirely different stories, two wildly different experiences living with HIV. There are nearly as many responses to medications as there are people living with the virus, and therein lies the challenge. With no new meds coming down the pike, researchers are looking to existing drugs for new ways to fight a disease that has already claimed 25 million people.
Now, 14 years after the introduction of protease inhibitors -- the first class of effective AIDS fighters -- the emphasis has shifted, in the words of Rowena Johnston, Ph.D., vice president and director of research at amfAR, the Foundation for AIDS Research, to "shifting drugs around to see what works best." Similarly, after years of despair, a recent large-scale clinical study in Thailand (more on that below) has shown that the same combination approach may bring a long-awaited vaccine to prevent HIV infection.
Like everyone else, amfAR is ultimately interested in a cure, but until then, the goal is to bring a patient's viral load down to undetectable levels.
"There has been concern about the fact that the near-time pipeline for investigational medications is not very robust right now," says W. David Hardy, MD, chief of the infectious diseases division at the David Geffen School of Medicine at the University of California, Los Angeles. But Hardy, who was treating patients before the advent in 1987 of the first AIDS drug, AZT, sees the new approach to fighting HIV as a cause of optimism.
The reason is the introduction of two new classes of drugs in recent years -- the first since the protease cocktail: integrase inhibitors and entry inhibitors. As their names imply, these classes of drugs inhibit HIV from entering healthy T4 cells, but each attacks a different aspect the virus's genetic makeup.
Faced with what Hardy calls "an embarrassment of riches," thanks to all of the new medications that have come on the market in recent years, researchers are still sorting out how to use all of these drugs to fight specific AIDS-related infections and eventually bring a patient's viral load as close to zero as possible. "We now have adequate drugs for almost every patient," Hardy says. And the availability of so many options, provided patients have access to medicines, means more ways to prevent or fight the onset of nasty side effects like kidney stones and lipodystrophy, and reactions like the dreaded "crix hump" and "crix belly," the disfiguring body alterations that bedeviled so many patients on protease inhibitors. The drugs are also making once-common AIDS-related diseases like PCP (a form of pneumonia) and Kaposi's sarcoma (cancer) a thing of the past. "Thank goodness, we don't see many opportunistic infections anymore," says University of Kansas professor Donna Sweet, MD.
There is also cause for optimism in the change in attitude in Washington, D.C. Everyone involved in HIV, from social workers to lab specialists, is expressing relief that President Obama has scrapped abstinence-only programs and restrictions on federal funding for embryonic stem-cell research, but it's unknown whether any of the economic stimulus money will make its way to AIDS research.
"I am very involved in HIV research, and I haven't truthfully heard about that much of a budget increase," says Margaret Hoffman-Terry, MD. As both professor at the Pennsylvania State University College of Medicine and chief of HIV medicine at Lehigh Valley Hospital in Allentown, Pa., Hoffman-Terry brings two perspectives to government funding -- clinical research and on-the-ground client services. Unfortunately, running a clinic for 700 indigent patients has made her less, not more, optimistic about finding the necessary funds to take care of patients with AIDS.
"Obama's election brought hope, but all of the funding remains at a flat level," she says. "Certainly opening up stem-cell research is very exciting. But people are worried about what the new health plan means to them. When you're on HIV meds, you're on them for life."
"We as scientists and virologists initially underestimated how diabolical HIV is," Hardy says. Since the discovery of HIV in 1984, researchers have been looking for a magic bullet that would prevent HIV from infecting the healthy, but the rapidly mutating virus has eluded efforts at developing a vaccine. Now, however, there's cause for renewed optimism. This fall came the results of the Thai study, the first in which a vaccine procedure showed real promise in the fight to eradicate AIDS.
Over 8,000 people received a combination "prime-boost" of two vaccines: one to prime the immune system to fight HIV, the other to strengthen the response. Another 8,000 people were injected with placebos. New infections occurred in 51 people who got the vaccine, compared to 74 who got the placebo. Even a one third drop in such a small sample gives researchers like Hardy "cautious optimism."
Then, only a few days after the Thai results were publicized, a network of researchers announced a new study to take place in 12 U.S. cities that will use a similar prime-boost strategy. "The idea with combination vaccines is to boost different arms of the immune response," says Richard Novak, MD, a researcher at Chicago's Project WISH and one of the prime movers in the study. This one will involve a much smaller sample, and only of sexually active gay men, because, as Novak explains, "Gay men just remain at a higher rate of infection."
Biotech company GeoVax, meanwhile, is conducting human trials of its own vaccine, which it believes could not only prevent HIV transmission but also help those already infected avoid progression to AIDS. So far, the vaccine largely prevented viral transmission in a trial involving monkeys, and the virus that did emerge was less virulent. And Canadian researcher Chil-Yong Kang has announced plans to test his vaccine on animals in the United States. Like Jonas Salk's polio vaccine, Kang's uses an entire dead virus and genetically engineers it so it can be produced in large quantities. HIV vaccines have generally used only a small amount of the virus's genetic material.
Researchers are looking closely at the widely reported case of a German man whose bone-marrow transplant cured him of his HIV two years ago. The man, being treated for leukemia, was treated with stem cells from a donor with a genetic mutation that provides resistance to HIV. But the high risk of mortality and the extreme unlikelihood of difficulty finding a donor with compatible tissue and who possesses that rare genetic trait made that case more sensational than immediately promising.
On another hopeful front, a microbicide was found to reduce HIV transmission by 30% in women who participated in a study in Africa and the United States. Although that's below the one-third threshold required by government agencies for general use, it's still the first gel, foam, or cream found to prevent HIV. Rectal use remains untested.
In spite of these advances, medicine that will prevent HIV seems to remain far in the future. Even the Thai study uses two meds that are already considered inferior to new drugs beginning to wend their way through the pipeline, so for now the emphasis remains on education and treatment. Today, most people who die of AIDS complications in the developed world are those who didn't get tested in time for effective treatment or who neglected to take their meds regularly.
Hoffman-Terry points out that doctors are wrestling with the problems of HIV-infected patients growing old -- something that would have unthinkable 15 years ago. "There's a new field of geriatric HIV," she says. "It's striking to think you've gone from a rapidly fatal illness to discussing old age for these patients."
Meanwhile, people like Rosen and Reigel continue to live day by day in the hope that new drugs, combinations of existing ones, and innovative treatment therapies will help them stay healthy and even eradicate the virus from their bodies entirely. And the rest of us -- the "worried well," as HIV-negative gay men were called in the 1980s -- look to a vaccine that will finally eliminate AIDS forever.
From our Sponsors
Most Popular
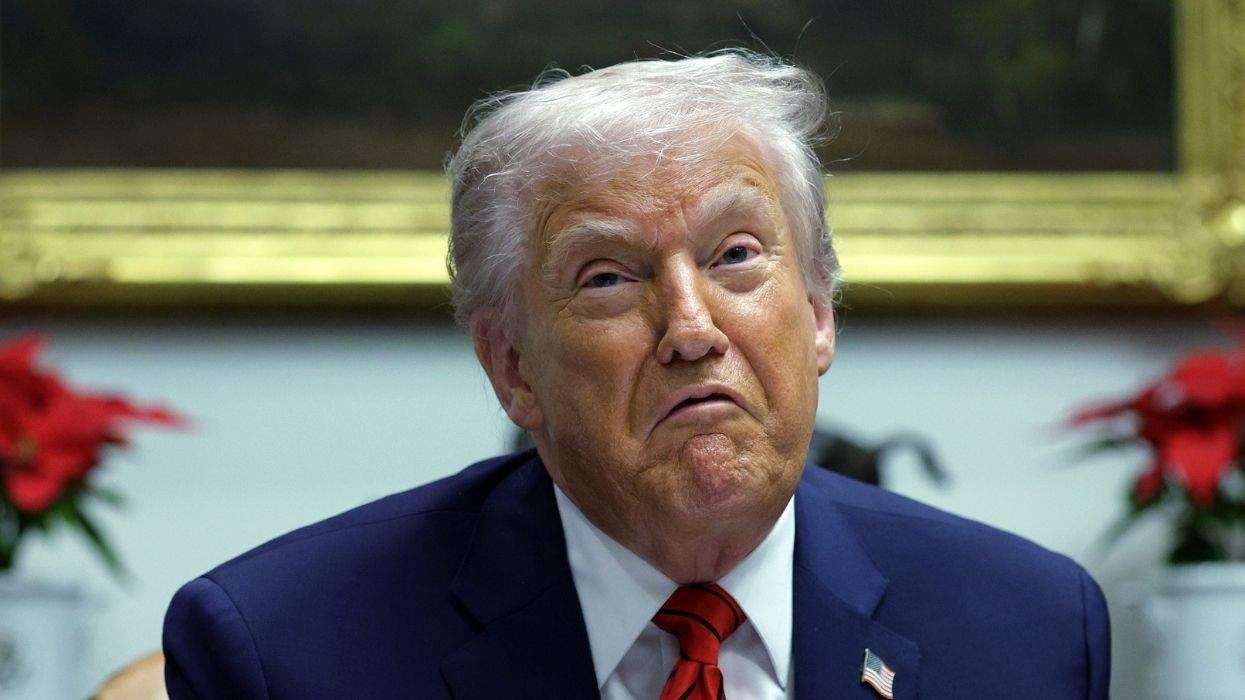
Bizarre Epstein files reference to Trump, Putin, and oral sex with ‘Bubba’ draws scrutiny in Congress
November 14 2025 4:08 PM
True
Jeffrey Epstein’s brother says the ‘Bubba’ mentioned in Trump oral sex email is not Bill Clinton
November 16 2025 9:15 AM
True
Watch Now: Pride Today
Latest Stories
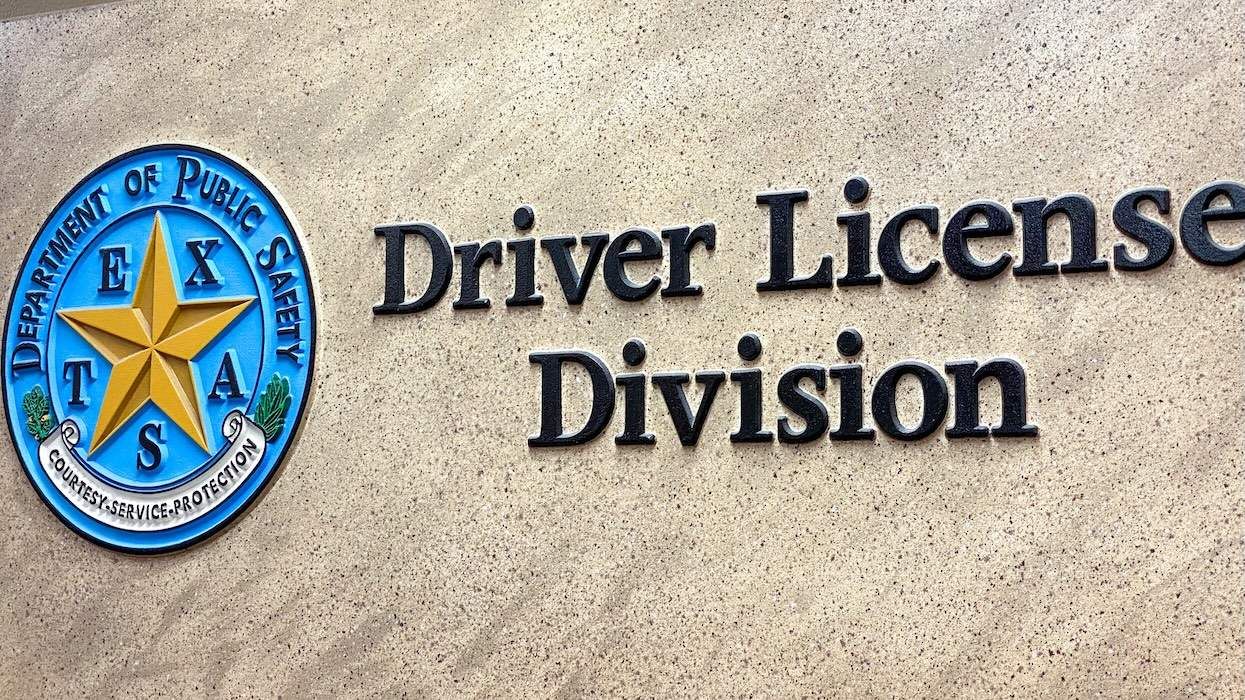
Is Texas using driver's license data to track transgender residents?
December 15 2025 6:46 PM
Rachel Maddow on standing up to government lies and her Walter Cronkite Award
December 15 2025 3:53 PM
Beloved gay 'General Hospital' star Anthony Geary dies at age 78
December 15 2025 2:07 PM
Rob Reiner deserves a place in queer TV history for Mike 'Meathead' Stivic in 'All in the Family'
December 15 2025 1:30 PM
Culver City elects first out gay mayor — and Elphaba helped celebrate
December 15 2025 1:08 PM
Texas city cancels 2026 Pride after local council rescinds LGBTQ+ protections
December 15 2025 12:55 PM
North Carolina county dissolves library board for refusing to toss book about a trans kid
December 15 2025 11:45 AM
Florida and Texas launch 'legal attack' in push to restrict abortion medication nationally
December 15 2025 11:18 AM
No, Crumbl is not Crumbl-ing, gay CEO Sawyer Hemsley says
December 15 2025 10:12 AM
11 times Donald Trump has randomly brought up his ‘transgender for everybody’ obsession
December 15 2025 9:22 AM
The story queer survivors aren't allowed to tell
December 15 2025 6:00 AM






























































Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes