Here To Inspire
Could Stem Cells Cure AIDS?
By continuing to use our site, you agree to our Private Policy and Terms of Use.
Researchers at the University of California, Los Angeles, made an astounding announcement Monday -- stem cells could be engineered to target and kill HIV. In an interview with Advocate.com, Scott Kitchen, assistant professor of medicine at UCLA's David Geffen School of Medicine, talks about the technology that made this discovery possible and how close these findings lead us to a vaccine.
How do the stem cells work against HIV?
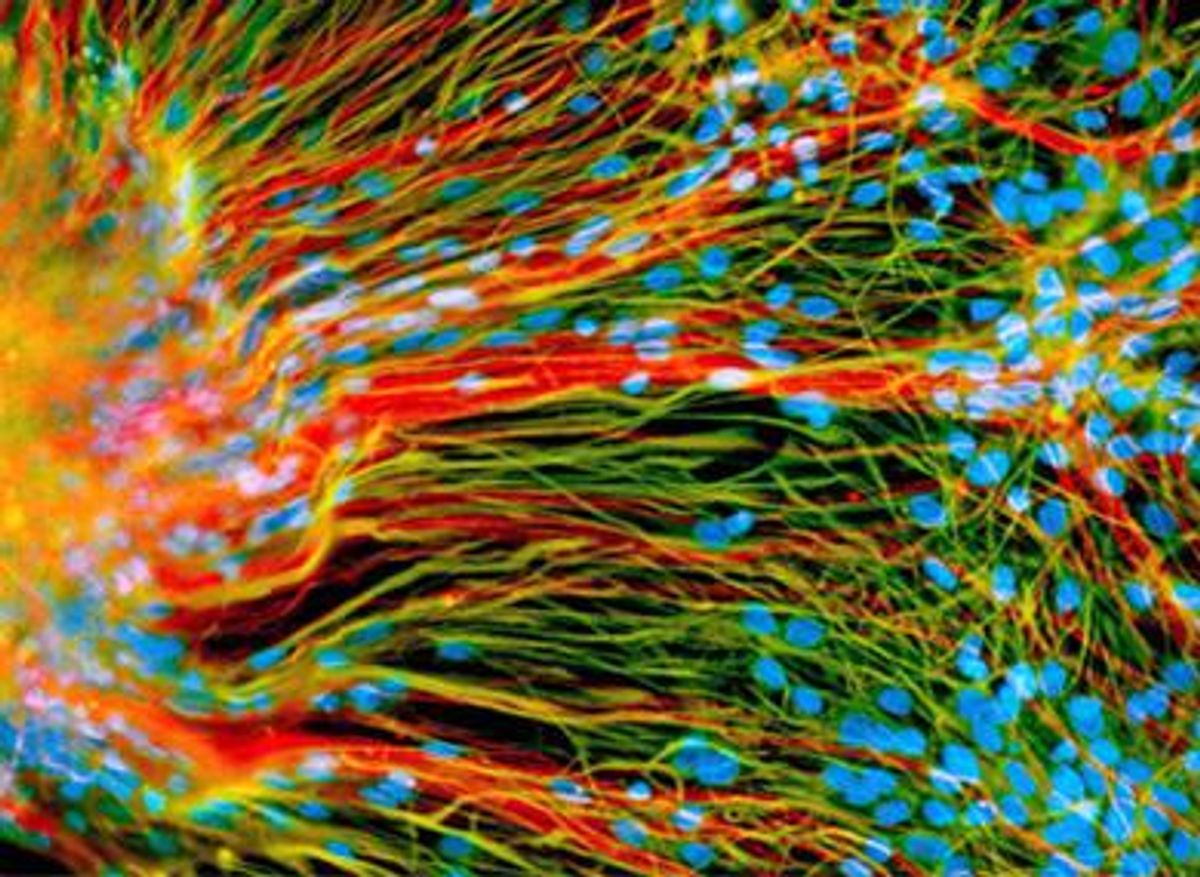
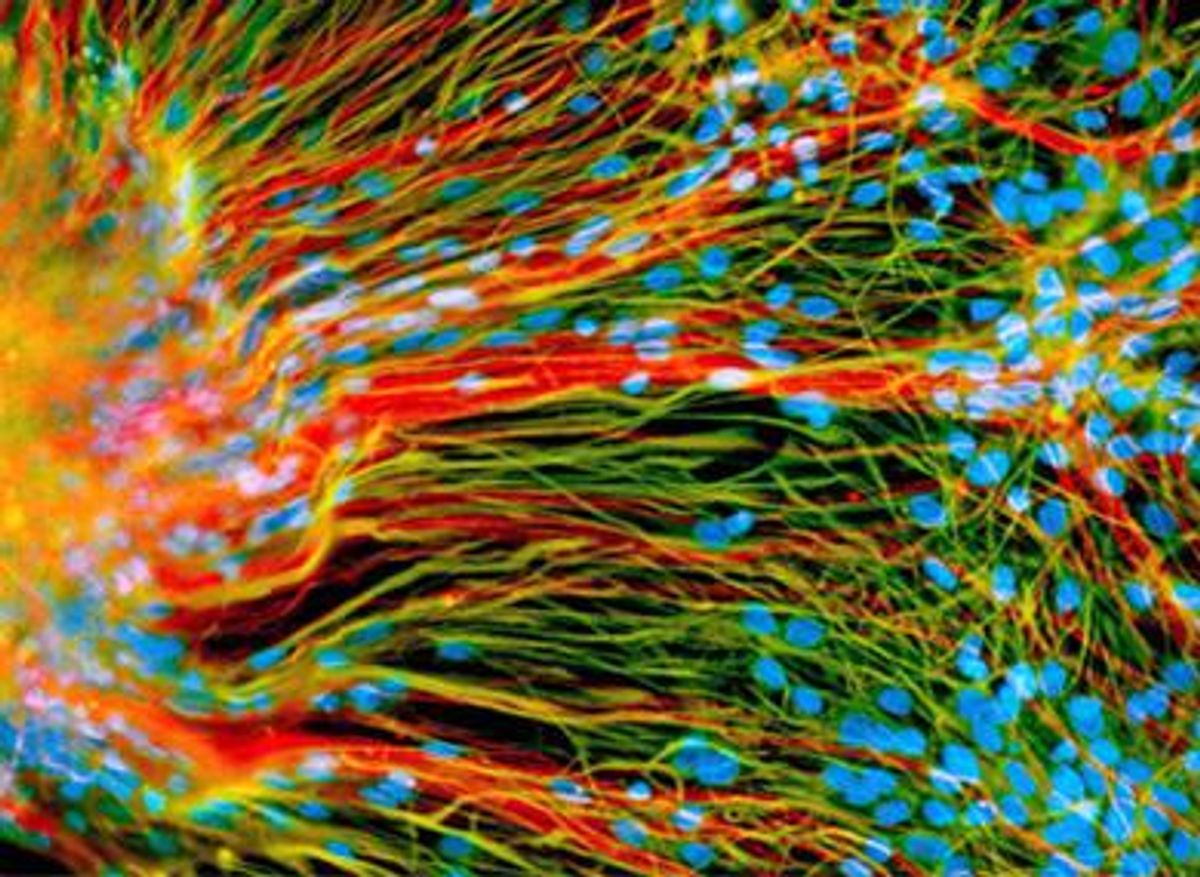
As you know, HIV is a lifelong infection. The immune system of a human is capable of responding to the virus and having an effect on its ability to replicate within the body, but ultimately it fails to clear the virus from the body, versus influenza or cold viruses. So what we were looking to do was find ways to restore the immune response in HIV-affected people in a way that specifically targets HIV itself. So we took cells from the blood of HIV-infected people -- people who have an ongoing infection but [not enough T] cells to completely eliminate the virus from the body. We took the cells that were there, identified a specific cell and a specific molecule on that cell that targets the cell toward HIV. So we molecularly cloned that molecule and took stem cells from another tissue source, another donor. This tissue is basically blood stem cells, and we engineered those blood stem cells ... to target HIV infection.
In order to test this in a living system, the genetically modified stem cells were placed into tissue that had been implanted into a mouse. This allows us to study the effects of the development of the stem cell into a mature T cell that is targeted to HIV in a living, breathing organism. In this model, we established this procedure allows the development of HIV-specific cells. So, the next step is to expand this into a system that allows us to examine the effects of these cells on HIV replication in vivo -- basically another animal-based system that allows us to look at the effects of these types of cells, these targeted HIV-specific cells, in eliminating the virus or lowering viral infection.
Was it previously believed that stem cells could destroy HIV, but it just wasn't proven?
There have been studies performed with mice cells that showed you can [alter and clone mice cells so they could battle] various mouse viruses. It was unknown whether you could perform this with the human system. The big advancement here is that you can. You can genetically engineer human blood stem cells to develop into T cells that specifically target HIV.
When did this study begin?
About three years ago as a concept. It really took off about a year ago as the technology became more and more conducive to allow the molecular cloning of these molecules.
So the technology made this advancement possible?
The technology to clone these T-cell receptors had been really a challenge prior to the current study. We've managed to more efficiently identify these molecules.
Would the next model system be human?
It will likely be another mammalian system to establish further efficacy -- to see if this really works robustly in a living breathing system.
So human testing is a way off?
Yes, because FDA requirements for a Phase I clinical trial requires a pretty good amount of preclinical development, and we're currently in that preclinical stage.
When will the next in vivo testing will happen?
It's in development right now.
If this vaccine does prove successful in future test subjects, could this be offered as a preventive vaccine, or would you have to be HIV-positive for it to work?
It's actually a reverse vaccine. A vaccine is where you give a person something and their immune response generates immunity to whatever they were given. This [advancement] engineers the immune cells in the individual to be targeted toward a specific thing like HIV. It wouldn't necessarily require HIV infection at the time of treatment -- high-risk people, for instance, could be provided this [as treatment] -- but we think it would be more efficacious in trying to eliminate the virus from the bodies of HIV-infected people.
If it was given to someone before they had the disease, would they have the necessary cells to battle the virus should they be exposed to it?
We really don't know at this point, but theoretically that's possible.
What kinds of stem cells were used in the research?
We used either fetal tissue-derived or core blood-derived stem cells. They're virtually identical to adult blood stem cells. We are postulating additional research to look into the feasibility of using embryonic-derived stem cells to engineer this approach but that's currently ongoing.
California allows stem cell research, but is there a worry about the controversial use of embryonic stem cells?
We don't believe so because we're predominantly using cells that already matured into a blood-forming stem cell unit, so they're not necessarily embryos or anything of that nature. Currently, what we're doing is utilizing the same type of approach that's utilized in bone marrow transplantation and tissue transplantation.
Would all the work you've done not been possible when Bush-era restrictions on stem cell research were in place?
Due to its use of blood-forming stem cells, it wouldn't be so much hindered. But overall, the kind of atmosphere is a lot more conducive to facilitating this type of research. The study was funded by the California Institute for Regenerative Medicine; the Proposition 71 money. Due to the passage of Proposition 71, the environment in California has been highly conducive to the success of this work.
What's the response been from the medical community?
The response has been very positive; [the findings have] a lot of potential to allow the development of therapeutics, not just for HIV but for other viruses that cause chronic infections in humans -- like hepatitis B, hepatitis C, herpes viruses, and papillomaviruses -- that the human immune system is in itself incapable of clearing. In addition it can be expanded to work involving cancer and tumors. But the scientific community in general has met the [research results] with a high degree of interest. This is really the first time this type of approach and this type of technology has been utilized in human tissue.
How hopeful are you that this will lead to a vaccine?
Very hopeful.