CONTACTAbout UsCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Equal Entertainment LLC.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
We need your help
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
Imagine if you could chuck your daily supply of anti-HIV meds and replace them with a monthly transfusion at your physician's office or, if possible, even a single shot that you give yourself. A small but determined group of biotech companies are researching new therapies that would last in the body for weeks or longer.
TaiMed Biologics and Progenics Pharmaceuticals, for example, are each looking into drugs known as monoclonal antibodies; these have already revolutionized cancer treatment and have made some chemotherapy far more tolerable when it comes to possible side effects. TaiMed's agent is an antibody that blocks HIV's attachment to the CD4 coreceptors. It is made by injecting mice with those same coreceptors, harvesting the natural antibodies the mice produces as a reaction, and then altering the DNA of those antibodies so that they are 99% human. Infused into an HIV patient, these antibodies, it's theorized, could last up to a month.
Progenics is in clinical trials of PRO 140, a monoclonal antibody that blocks the CCR5 coreceptor. Study results published this year indicated that once-weekly and every-other-week subcutaneous injections of the antibody both suppressed viral loads significantly, and patients could potentially administer the injections themselves. PRO 140 has received fast-track designation from the Food and Drug Administration.
Tibotec Pharmaceuticals, the antiviral division of Johnson & Johnson, is attempting to produce a long-acting version of one of its upcoming nonnukes, currently referred to as TMC278. The medication is processed to create a mixture of tiny particles of TMC278 with a liquid to create a solution called a nanosuspension. When injected into the body this solution works to extend the release of medication over the course of weeks.
Another compound, EFdA, a nucleoside reverse transcriptase inhibitor being developed in academic and National Institutes of Health labs, meanwhile, has shown itself to be extremely powerful in both test-tube and primate studies.
"This new compound is 60,000 times more potent than any other drug that is currently being used to treat HIV," says Stefan Sarafianos, an assistant professor of microbiology and immunology at the University of Missouri school of medicine. "This compound has a different chemical makeup than other approved therapies and creates an exceptional amount of antiviral activity. It's activated very quickly and stays long in the body to fight the virus and protect from infection."
Curiously, the EFdA compound was discovered by a soy sauce manufacturer in Japan that was developing it as a flavor enhancer. The company's product tests eventually found it had antiviral capabilities. With a half-life of three weeks, EFdA could be taken less often than currently available options. It also has shown potential for use in a microbicide.
But there's a major question yet to be addressed: Can researchers develop enough of these long-lasting medications to piece together a viable full cocktail? After all, currently successful combination therapies contain at least three compounds -- whether in the form of three drugs taken together or combo pills taken with one or more additional meds -- since each attacks HIV in different points of the infection cycle.
That's not to say, though, that they won't have their benefit. "I see these long-acting drugs as a potential answer to adherence problems," says Jeffrey Jacobson, the cochair of the long-acting drug task force for the AIDS Clinical Trials Group.
With this type of treatment breakthrough possibly becoming available in the next few years, HIV Plus decided to check in with experts to see what other advancements they think could be in store for HIVers over the decade ahead. And of course, we're looking at the current traditional treatments that are working their way through clinical research.
While drugmakers have produced 30 individual or combination antiretrovirals since 1987 (28 of which are still on the market) the federal Food and Drug Administration hasn't approved any new medications since the nonnucleoside analog Intelence (etravirine) in 2008. Although output from the new-drug pipeline has slowed, manufacturers are still looking for medications that have fewer side effects, are better at fighting resistance, and reduce pill burden. Companies are racing to develop a once-a-day combo pill for treatment-naive HIVers that is as effective or more effective than Atripla but that has fewer side effects, providing an alternative for people who are troubled in particular by Atripla's tendency to cause vivid dreams -- a side effect attributed to its Sustiva (efavirenz) component.
But even though there has been no new antiretroviral released to the market for almost two years, there are a dozen or so anti-HIV candidates currently in advanced clinical studies (Phase II and III). If they make it through these stages, at least six compounds could be submitted for Food and Drug Administration approval in the next few years.
> Bevirimat, a maturation inhibitor being developed by Panacos and purchased by Myriad Genetics, showed mixed results in Phase IIb trials in 2007, working in only 60% of HIVers studied because of mutations in their respective viral populations.
> Elvitegravir is an integrase inhibitor being developed by Gllead; it's in Phase III.
> GSK-572 is an integrase inhibitor being developed by ViiV Healthcare, the combined antiretroviral development units of GlaxoSmithKline and Pfizer. Promising results from its Phase IIa trials were released in July 2009. If ultimately successful, this med could become an alternative to Atripla when combined in a daily dose with Ziagen (abacavir) and Epivir (3TC). Although there is an effective screening test to rule out those who would not tolerate the drug, the allergic reaction some HIVers have to Ziagen remains a barrier.
> The "Quad" is a once-a-day combo pill from Gilead that combines forthcoming integrase inhibitor elvitegravir, Truvada (Viread and Emtriva), and a new boosting agent that researchers hope will be better-tolerated than Norvir (ritonavir). Currently being studied in treatment-naive patients, with good results in Phase II trials, it could also become an alternative to Atripla.
> Rilpivirine (TMC278) is a second-generation nonnucleoside analog from Tibotec that entered Phase III trials in April 2008; study completion is expected in January. If successful, the new nonnuke may challenge Atripla if studies show it is as potent when combined in a single pill with Truvada.
> Vicriviroc is a CCR5 antagonist, being developed by Merck, that did not show promise for treatment-experienced HIVers; but Phase II/III studies are ongoing for people who have not previously been on treatment. A previous CCR5 inhibitor, Selzentry (maraviroc), was approved in 2007.
While none of these specific drugs promises to revolutionize treatment, over the coming decade, experts and pharmaceutical representatives say they anticipate even more combination pills will hit the market -- and not just formulations aimed mostly at treatment-naive HIVers. Otherwise, there are many other scientific endeavors still in their infancy that could one day drastically change how HIV is treated and possibly even lead to a cure. We may not see such total ground shift by the end of the decade, but there should at least be a better idea of where we're headed by then.
Cure Research
Long gone are the days when scientists believed extended suppression of HIV through highly active antiretroviral therapy could permanently eradicate the virus from the body. Elusive viral reservoirs continue to harbor small amounts of HIV and evade medications. Now, as new-drug development slows and researchers look to the next big thing, some of the more enterprising among them are trying to better understand these reservoirs -- what they are and how they manage to remain mostly untouched by treatment -- in order to one day perhaps purge those last remaining HIV cells from the body.
"Ten years from now I think we'll have made progress toward eradication," says Steven Deeks, an HIV researcher at the University of California, San Francisco. "I don't think anyone will have been cured. Hopefully by that time we'll be actively involved in clinical trials to try and cure HIV."
David Margolis, a professor of medicine, microbiology, and immunology at the University of North Carolina at Chapel Hill's school of medicine, whose research lab has been studying viral reservoirs for the past decade, says, "Progress has been very exciting in the past year or two because more groups are seriously looking at these questions of [whether it is] possible to eradicate infection or to treat someone in such a way that they don't have to be on chronic suppressive therapy."
The reservoir can mean different things to different scientists. In part, it is made up of resting memory T cells, which for some reason will stop replicating the virus and go into a kind of extended hibernation. During this time, antiretrovirals do not recognize that these T cells are infected with HIV. The challenge for researchers like Margolis is to provoke these cells to express the virus again.
"You could imagine a cure pack -- where you get diagnosed, and you go on antiretrovirals for six months to knock down your viral load to zero," says Bob Huff, a member of the Drug Development Committee at the AIDS Treatment Activists Coalition. "Then you take another series of pills to express all the residual HIV. Next, you stop that and follow up with a few more months of [antiretrovirals], and then you stop and see if it ever comes back or not. That counts as a revolution. That would be awesome."
There may be an additional type of cell -- or more than one -- that quietly harbors HIV, but researchers have yet to figure out this mystery. Also, HIV may hide from antiretrovirals in tissues that are inaccessible to the medications, such as the testes, brain, or lymph tissues.
AmfAR, the Foundation for AIDS Research, which prides itself on adopting maverick causes, has now put its weight behind cure research, making the cause the cornerstone of its research program with an initial $1.2 million round of funding. Rowena Johnston, vice president of research at amfAR, says that a "functional cure," in which a person still has HIV in the body but is able to control the infection without the use of ongoing drug therapy, could come from better understanding what are known as "elite controllers," the rare HIV-positive people who are somehow able to produce this effect on their own, without the aid of treatment.
Koronis Pharmaceuticals, a biotech company in Redmond, Wash., is working on a therapy that randomly inserts genetic errors into HIV's DNA as it replicates itself. If successful, this treatment, currently in Phase II clinical trials, would eventually lead to a "viral collapse," in which the entire HIV population is so riddled with errors that it is no longer able to infect new cells or pass from person to person. Jeff Parkins, vice president of clinical development at Koronis, says that as the reservoir turns over with time, the end result of the therapy could be a cure. Unfortunately, he adds, it's anybody's guess as to how long this would take. Ask one scientist the life cycle of the reservoir and he'll say six months. Ask another: six years. And even another: 60 years.
Other hope for the so-called functional cure comes from the many labs currently researching genetic therapies that would train the body to better fight off HIV. After harvesting a patient's T cells or stem cells that produce T cells, scientists are inserting genes that, for example, lack the expression for the CCR5 coreceptor that most HIV cells need in order to latch onto the T cells. They then return the cells to the body and hope that these HIV-resistant T cells will flourish and become the dominant aspect of the immune system. A major consideration of this line of therapy is the price tag -- since the process, still in its infancy, costs tens of thousands of dollars. However, if it were needed only twice a year, the savings in comparison to daily medications could tip the balance in its favor. Stopping Transmission
Science has advanced at a snail's pace in finding medications -- topical microbicides or oral preexposure prophylaxis -- that can prevent HIV transmission. Early studies of microbicides have informed further research, but they have so far failed to prove the agents can be effective.
Ian McGowan, a principal investigator of the Microbicide Trials Network, says the next few years will be sink or swim for microbicide research. If current studies show promise, a product may reach the market within 10 years, he predicts. Otherwise, all research will likely close up shop for good. "By 2020 we may have a toolbox," McGowan says. "It may have pills in it; it may have gels. Depending on people's circumstances, they may use one or the other, or they may use both."
A big conundrum with both microbicide and PrEP research is in developing a proper dosing schedule for a product that is both convenient and effective to use in advance of unpredictable sexual encounters. Antiretroviral agents may take up to 12 hours to activate after they're either ingested in pill form or placed in the vagina or rectum in a microbicide gel. One potential answer is the investigatory nucleoside analog EFdA, whose form mimics human cells, so it is recognized by the immune system and activated in only 15 minutes. Because it is so potent, it also lasts much longer than other antiretroviral agents.
Research is currently deducing whether administering a daily oral antiretroviral to high-risk HIV-negative populations can curb transmission. Assuming this method is effective, further studies will look to see if occasional doses -- a "disco pill," in McGowan's words -- are also effective. At that point, cost will become a major consideration. Will insurers pay? Will certain high-risk populations be willing to spend the money for such precautions? With luck, a successful drug would go off patent by 2020, allowing for cheaper generic versions and more widespread use.
Another option, however, is an occasional infusion of a long-acting HIV therapy, such as the potential nano formulation of Tibotec's TMC278 compound, which the company is hoping will work as PrEP. In theory, the drug would last long enough once applied to provide protection for a month.
Test and Treat
While the jury is still out, recent signs indicate that scientists are beginning to move toward a greater consensus that starting antiretroviral treatment earlier now outweighs the risks of long-term therapy. The San Francisco department of health has made "test and treat" -- getting HIV patients on therapy as soon as possible after diagnosis -- its recommended policy.
Even if T-cell counts remain at healthy levels for years, it seems that untreated HIV still harms the body, leading to a higher risk of conditions down the line, like heart disease, cancer, and kidney failure. A University of Washington study published in The New England Journal of Medicine in 2009 found a significant survival benefit for people who began treatment when their T-cell counts were still above 500.
And also in 2009 the first randomized, controlled trial to compare the risks and benefits of earlier versus delayed treatment, the National Institutes of Health's START study, began. The results of the study, expected by 2015, should finally provide a definitive answer to this long-running mystery. Additional research going on around the world will hopefully prove whether widespread antiretroviral treatment, by lowering overall "community viral load," can in turn reduce infection rates.
Aging Issues
By the middle of the decade half of all HIVers will be older than 50. As the population grays, research is putting its muscle behind trying to understand why HIV infection seems to lead to accelerated aging in long-term survivors. The research is particularly critical considering that, among the deaths in today's older HIVers, one third are due to non-AIDS-related causes.
A major culprit under study is what's known as immune inflammation, which has been shown to contribute to aging in non-HIVers. When any virus enters the body the immune system releases inflammatory cytokine cells. In the case of an ordinary flu, for example, these cells would help clear the body of the illness in a relatively brief period of time and would then retreat. However, in HIV patients this inflammation seems to last indefinitely and can cause major damage to other human cells. Antiretrovirals don't stop this effect because the body maintains its inflammatory response to the low levels of virus still replicating in reservoirs. The consequence is an elevated risk of many potentially fatal conditions associated with advanced age, including heart disease, osteoporosis, diabetes, muscle wasting, liver damage, and Alzheimer's.
The goal of research on this matter is twofold: First, to understand why HIVers have a higher incidence of age-related illnesses. And second, if inflammation is indeed a major source of the problem, to find some sort of anti-inflammatory agent that can tone down the body's overreaction to the low levels of virus. At-Home Monitoring
Keith Alcorn of London-based AIDS organization NAM predicts that by 2020 HIVers will be able to monitor their own viral load and CD4-cell levels at home and then report back electronically to their physician. This will mean fewer doctor visits and move the self-management of HIV closer to that of diabetes patients checking their glucose levels.
He also says affordable at-home rapid antibody tests should be widely available. Unfortunately, though, the "window period," when someone is infected with the virus but hasn't yet developed the antibodies that will lead to a positive test, will remain a problem. People testing themselves within this approximately six-week time frame won't be able to get a completely accurate read from a home viral-load test either, Alcorn believes, since those tests have a wide margin of error when detecting low levels of the virus.
Normal Life Expectancy
Brian Risley, a treatment educator at AIDS Project Los Angeles, predicts that HIVers will eventually have a normal life expectancy, thanks to improved treatments and better understanding of when to begin antiretroviral therapy. He points to a recent European study that found "near normal" survival for HIVers who kept their T-cell count above 500 for three years or more.
Reversing Lipodystrophy
There are few options for permanently reversing the effects of lipodystrophy -- the redistribution of fat throughout the body that is a side effect of some anti-HIV medications -- outside of expensive, temporary facial fillers. The FDA is on the verge of approving a drug called tesamorelin, which has been shown to cut deep belly fat deposits -- a.k.a. "Crix belly" -- by an average of 18%. APLA's Risley sees a time not far off when scientists will better understand the causes of lipodystrophy and can then reverse the condition through the use of statin and glucose-regulating drugs.
Health Care Reform
Today, three in 10 HIVers are uninsured. Forty-five percent have an income of less than $10,000, and 62% are unemployed. More than half receive health coverage through Medicaid or Medicare. Considering this portrait of the population, the passage of health care reform promises big changes for HIVers as the legislation is rolled out between now and its full implementation in 2014.
Robert Greenwald, director of the Health Law and Policy Clinic at Harvard Law School, applauds the bill. "While I certainly have some concerns and disappointments," he says, "there is no question that this health care reform bill represents a significant step forward in meeting the care and treatment needs of many, many people living with HIV."
Some of the major benefits this year:
>The infamous medication "doughnut hole" gap, during which beneficiaries have to pay out of pocket for prescriptions under the Medicare Part D prescription drug benefit, will phase out by 2020. Starting this year, the government will provide a $250 rebate. In 2011 brand name drugs will be 50% off, but their full price will still count toward the total doughnut-hole expenditures, potentially cutting out-of-pocket costs in half. AIDS Drug Assistance Program coverage will also count toward the doughnut hole.
>Temporary high-risk insurance pools will provide health insurance to people who have been shut out of coverage because of preexisting conditions for six months or longer.
>If you are 26 or under, you can still qualify for coverage under your parents' health plan.
>New insurance policies must provide coverage for annual checkups and preventive care, like cancer screenings.
>Lifetime benefit caps will end.
Some of the major benefits by 2014:
>All Americans must obtain insurance coverage.
>Anyone with an income of 133% or less of the federal poverty level will qualify for Medicaid (currently $14,403 for an individual or $29,326 for a family of four). A disability diagnosis (an AIDS diagnosis counts as one; an HIV diagnosis doesn't) will no longer be necessary.
>Underwriting and preexisting condition exclusions will end; insurers may not reject you or charge you a higher premium based on your health status.
>Government subsidies will help with premium costs for people with incomes up to four times the federal poverty level ($43,320 for an individual or $88,200 for a family of four).
>Plans will have to provide coverage for mental-health and substance-abuse treatment.
>Insurance exchanges will pool risk, allowing for more affordable individual or small-business health policies. This will reduce the likelihood of workplace discrimination based on HIV status if an employer is concerned an HIVer's medical bills may drive up premiums.
>HIVers will have more flexibility in where they live and how they work, since the availability and affordability of health benefits will no longer depend entirely on an employer's benefits package or a certain state's public-assistance budget.
However, there is a major drawback to health reform plan. By 2019, there will still likely be 23 million uninsured Americans, one third of whom will be undocumented immigrants. The rest will likely be members of hard-to-reach populations -- for example, the homeless -- who have not gotten themselves into the system. Depending on the political climate as the decade unfolds, the undocumented population may find itself increasingly squeezed out even from Ryan White Act sources of medical funding.
From our Sponsors
Most Popular
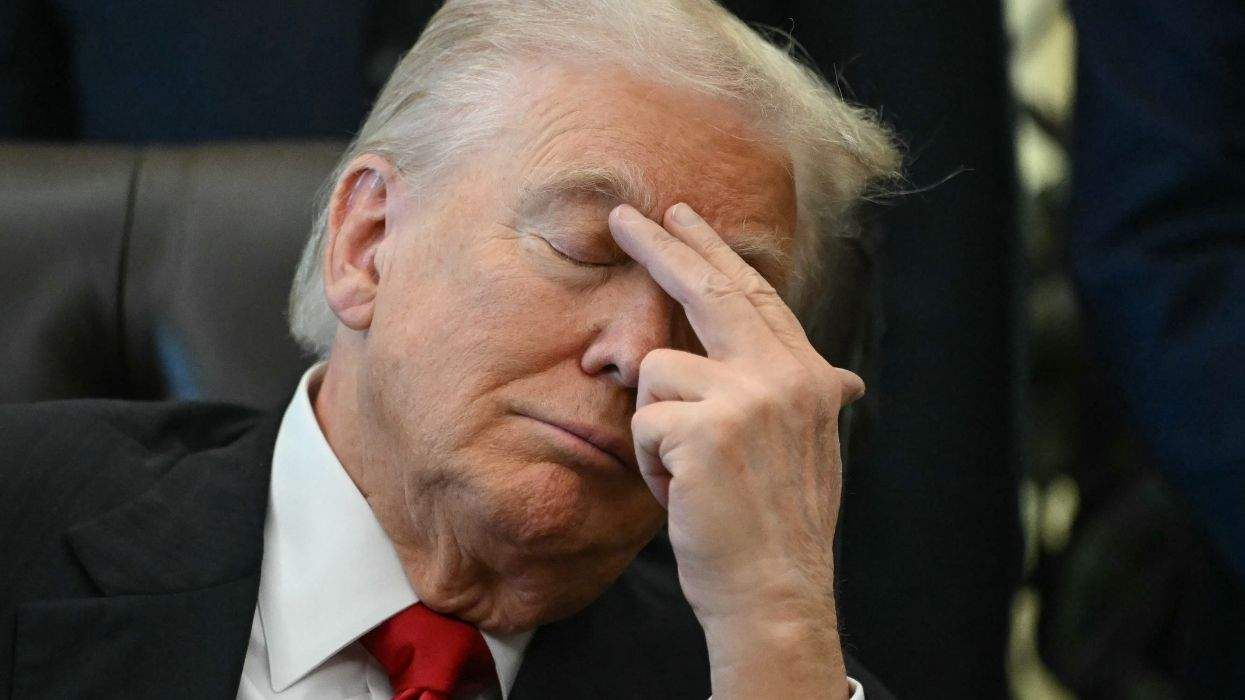
Bizarre Epstein files reference to Trump, Putin, and oral sex with ‘Bubba’ draws scrutiny in Congress
November 14 2025 4:08 PM
True
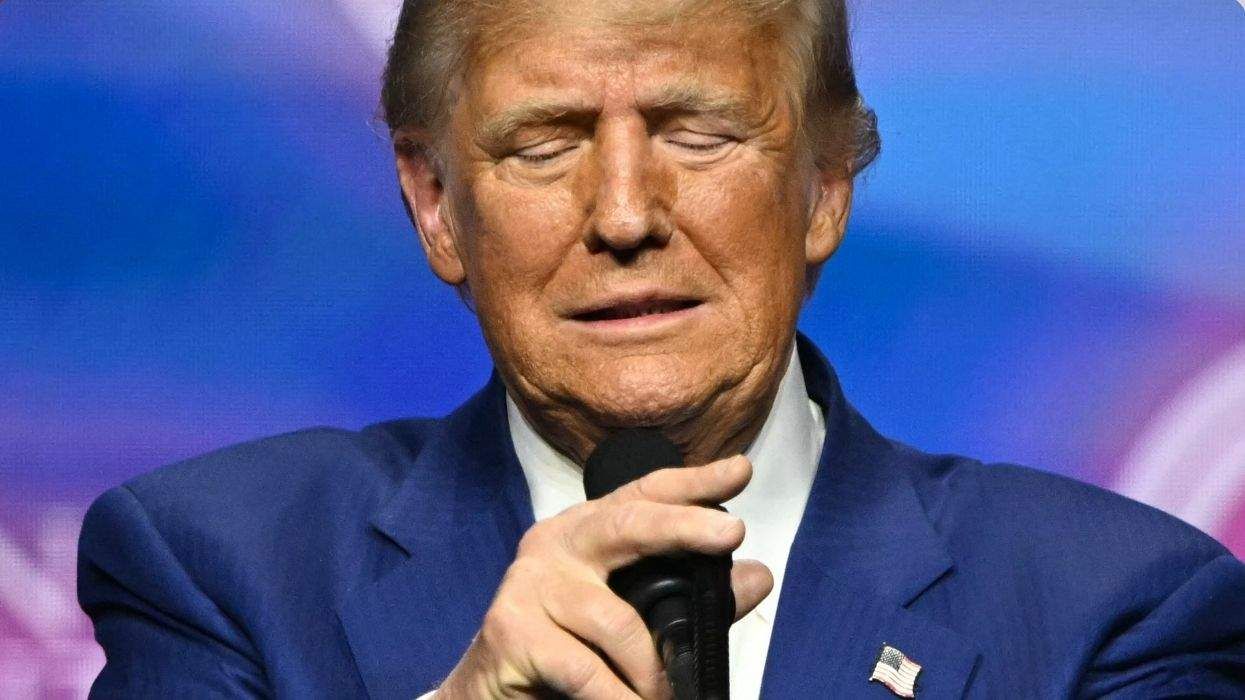
Jeffrey Epstein’s brother says the ‘Bubba’ mentioned in Trump oral sex email is not Bill Clinton
November 16 2025 9:15 AM
True
Watch Now: Pride Today
Latest Stories
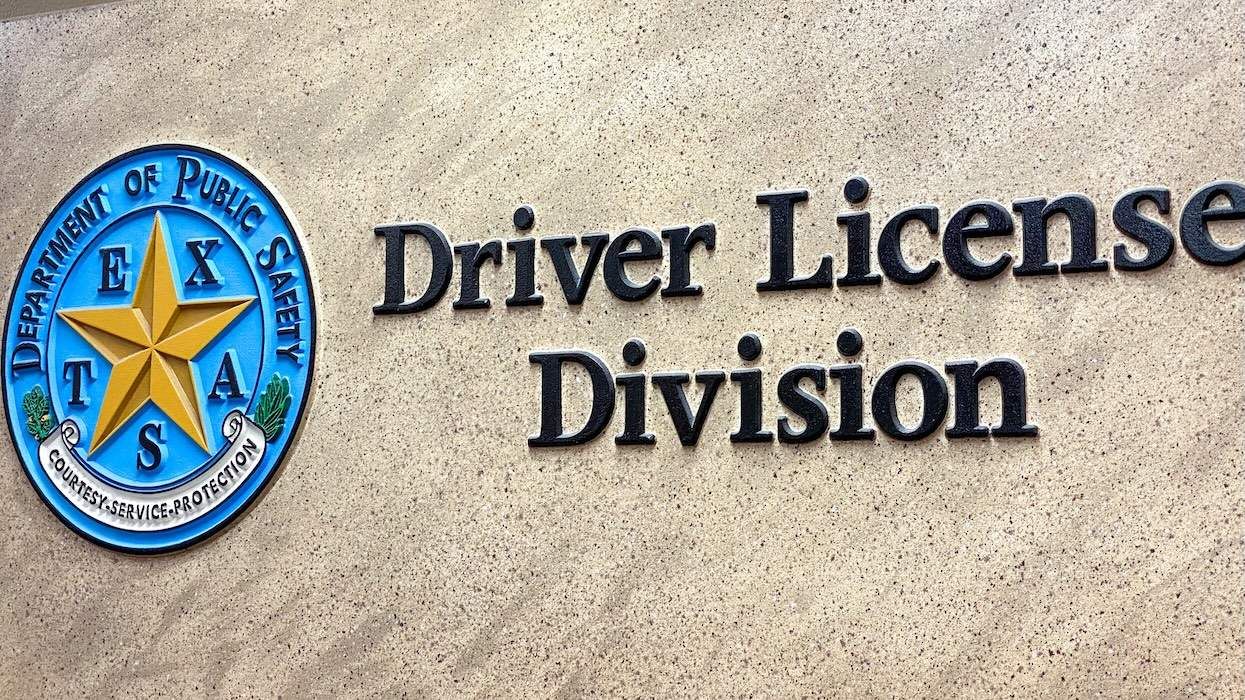
Is Texas using driver's license data to track transgender residents?
December 15 2025 6:46 PM
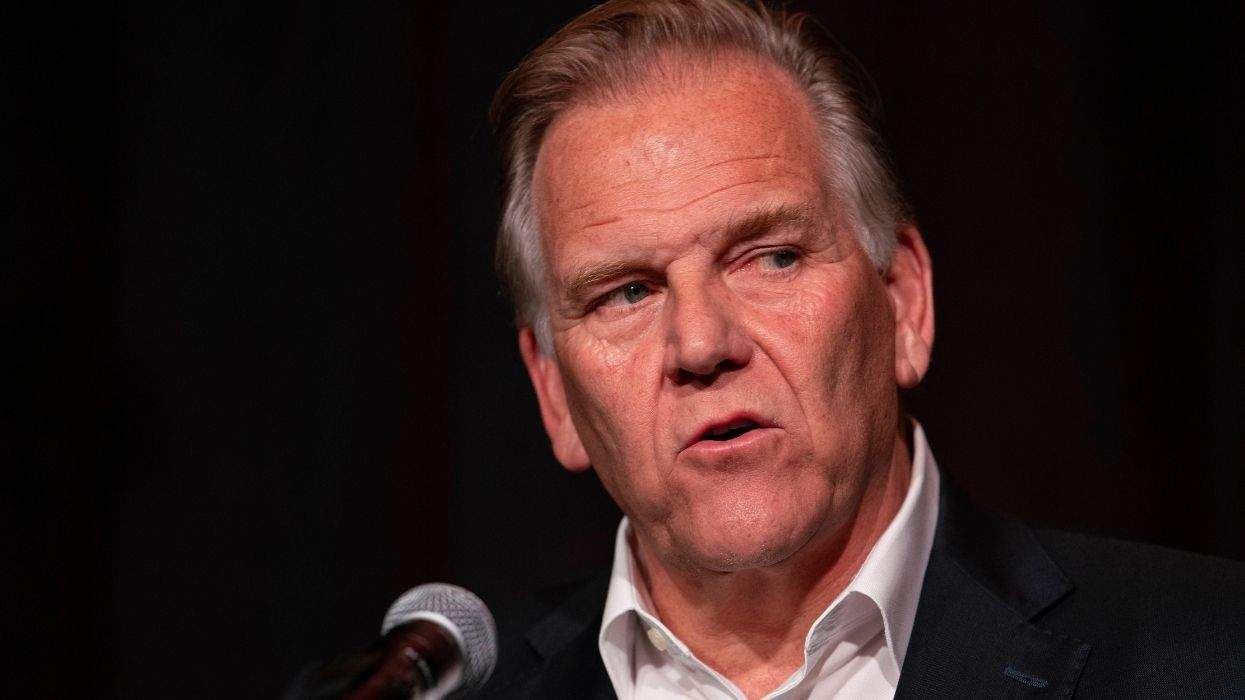
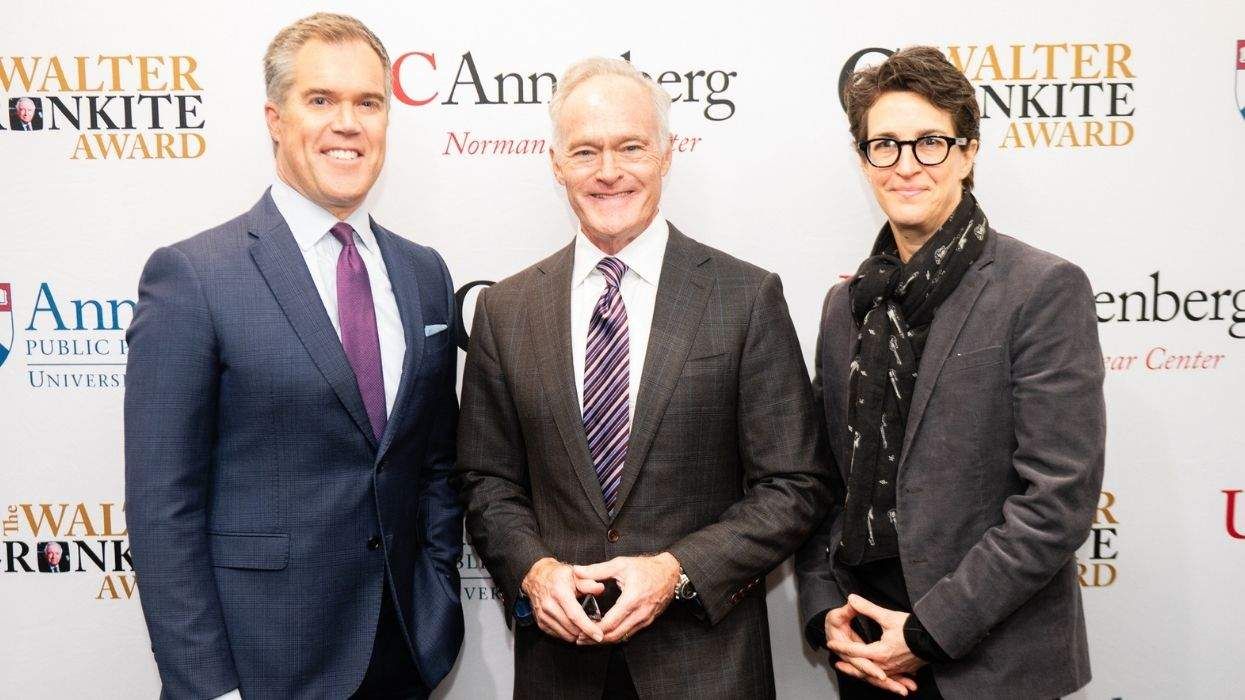
Rachel Maddow on standing up to government lies and her Walter Cronkite Award
December 15 2025 3:53 PM
Beloved gay 'General Hospital' star Anthony Geary dies at age 78
December 15 2025 2:07 PM
Rob Reiner deserves a place in queer TV history for Mike 'Meathead' Stivic in 'All in the Family'
December 15 2025 1:30 PM
Culver City elects first out gay mayor — and Elphaba helped celebrate
December 15 2025 1:08 PM
Texas city cancels 2026 Pride after local council rescinds LGBTQ+ protections
December 15 2025 12:55 PM
North Carolina county dissolves library board for refusing to toss book about a trans kid
December 15 2025 11:45 AM
Florida and Texas launch 'legal attack' in push to restrict abortion medication nationally
December 15 2025 11:18 AM
No, Crumbl is not Crumbl-ing, gay CEO Sawyer Hemsley says
December 15 2025 10:12 AM
11 times Donald Trump has randomly brought up his ‘transgender for everybody’ obsession
December 15 2025 9:22 AM
The story queer survivors aren't allowed to tell
December 15 2025 6:00 AM




























































Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes