IN JULY 1981, the Centers for Disease Control noted that five gay men in Los Angeles had fallen victim to an uncommon strain of pneumonia. A brief buried inside the Morbidity and Mortality Weekly Reportconcluded, "All the above observations suggest the possibility of a cellular-immune dysfunction related to a common exposure that predisposes individuals to opportunistic infections." And so began the official record of HIV and AIDS in the United States. Epidemiologists would later identify sexual contact and sharing needles as the chief "common exposures."
University of Chicago professor of medicine Renslow Sherer, then a physician at Cook County Hospital, knew it was only a matter of time before someone would appear in Chicago with the symptoms. In 1982, a young man who could no longer complete his daily eight-mile run came to the hospital with an uncommon strain of pneumonia. As more symptomatic gay men, Haitians, and injection drug users turned up, Sherer and Ron Sable, a gay physician who would later die of AIDS, started a clinic to treat them.
Due to exponential growth in need, it expanded the next year. There were 140 patients by 1986 and 1,400 more in the four following years. "We guessed that it was going to rise that way, but we didn't know," Sherer said. "Much more painful was the obvious morbidity and mortality. Everybody died in those early days."
In 1987, AZT became the first antiviral medication approved to treat HIV and AIDS. Single- and double-drug therapies were introduced but only added 12 to 24 months of life expectancy. "They were helpful and kept people alive, but only for a while," said Sherer. This continued until 1996, when researchers at the Vancouver AIDS Conference announced the effectiveness of protease-inhibiting multidrug therapy. Today, regimens suppress the virus and stabilize T cells, and people living with HIV. generally enjoy near-normal life expectancies.
Sherer says it is difficult but necessary to think about the wanton destruction of the AIDS epidemic "partly because of the complacency that's out there now. ... People say, 'It's not as bad as it once was,' but it's still a dreadful disease. It's not anything that you'd want, and the fact that we now have new means to prevent HIV and limit new infections with treatment as prevention for everybody who's positive and pre-exposure prophylaxis for everyone who's negative is really key."
By 1994, epidemiologists knew that the presence of AZT alone in HIV-positive pregnant women was correlated with a significant reduction in the odds of viral transmission to their children. Two- and three-drug antiretroviral therapies (ART) further reduced the odds. There are no confirmed cases of positive, seronegative individuals receiving three-drug ART spreading the virus -- last year, the CDC confirmed that maintaining an undetectable viral load makes one unable to transmit HIV. When medical workers suffered needle-stick injuries, a course of ART.became standard to prevent acquisition of the virus -- post-exposure prophylaxis (PEP) became more effective as drug regimens became more effective.
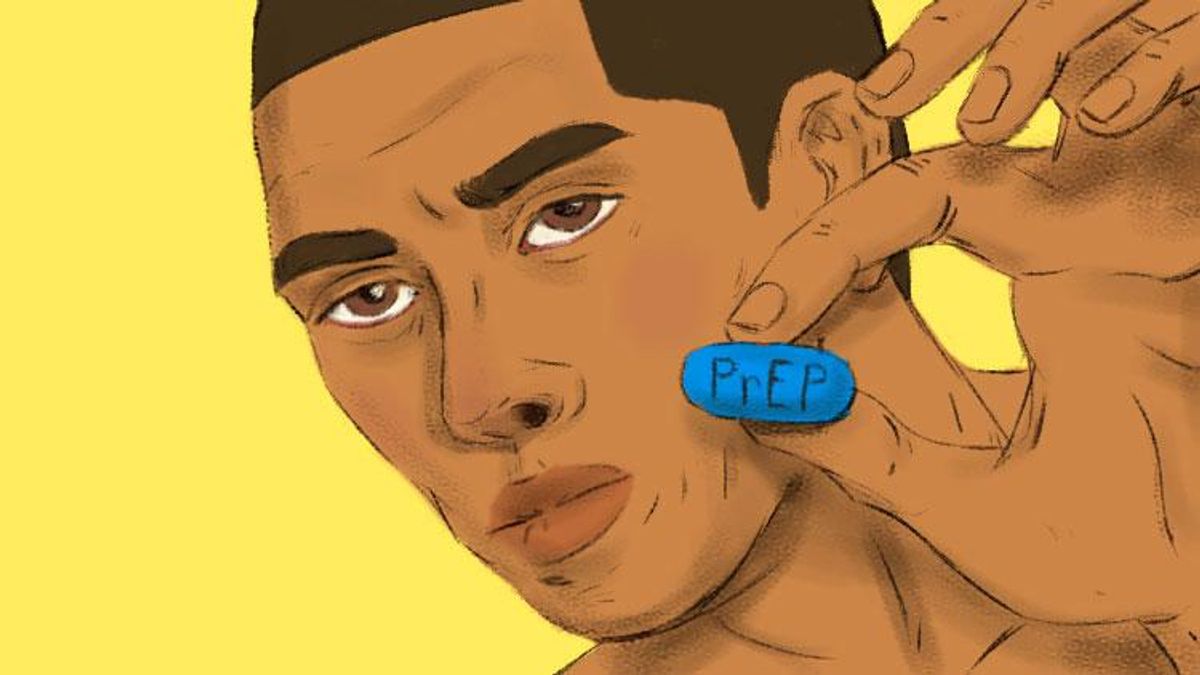
PEP's theoretical explanation suggested that pre-exposure prophylaxis, or PrEP, was a theoretical possibility. Researchers who first administered ART to macaques before exposing them to simian immunodeficiency virus saw that the odds of infection were strongly reduced. Human clinical trials began in 2010 and showed promise for both men and women. Initial adherence was "sketchy," in Sherer's words, but those that took their drugs saw an efficacy of over 90 percent.
In 2012, the Food and Drug Administration approved emtricitabine/tenofovir, sold under the trade name Truvada by Gilead Sciences, for PrEP.
I myself was born in 1992 and came out at 14. My mother says she felt concern about HIV as I entered adolescence: "It was new territory for me, because I just had to worry about pregnancy with your siblings. With you, I was worried about your life." I firmly associated condoms with not contracting HIV from the time I became sexually active.
At college in the Bay Area, I noticed more and more guys saying they were on PrEP on their Grindr profiles. The World Health Organization recommended in 2014 that all HIV-negative men who has sex with men (MSM) take PrEP, and I asked my primary care provider at home in liberal Bloomington, Ind., to prescribe it for me. She refused. Only one of her other patients had requested it, and he and his boyfriend wanted an open relationship. "Anyway," she said, "I haven't done my research on it." She followed up with something about the potential for liver damage.
I spent the first year after college cohabiting with someone in Minneapolis and didn't feel the need to start PrEP, though the Minnesota AIDS Project strongly recommended it when I got tested there. I moved to Chicago alone in 2016 to start graduate school. I had used condoms with literally every nonromantic sexual partner up until that point, and then I didn't. And that's when I knew it was time.
I called the University of Chicago Medical Center to make an appointment. One day in early November, Renslow Sherer asked me why I was there to see him.
"I'm a man who has sex with men," I said buoyantly, "and I want to get on PrEP."
"That is an excellent reason to have come in today," he replied.
I took the first pill the day after the election.
PrEP is driving a paradigm shift of queer life in the United States, but the revolution's parameters are complicated. We are not witnessing the end of HIV and AIDS in the United States -- queer people, especially queer people of color, are still contracting the virus at disproportionate rates, and people still die of AIDS.
But the science is clear: people around the world take Truvada for PrEP because it prevents HIV infection. A 2015 Kaiser Permanente study of 600 high-risk individuals found that none of them contracted HIV over the 2.5 years they were observed taking PrEP. Studies have shown that even nondaily adherence to the regimen provides a strong degree of protection. Sherer says PrEP users in France only take a pill four times a week and references this to answer those who dispute PrEP's utility in public health efforts because some patients do not take it as directed. (He still advises his patients to take Truvada every day.) "Disco dosing" -- taking PrEP only around periods of riskier sexual behavior -- has entered the gay lexicon.
Go on Grindr or Scruff in any large American city and see scores of queer people who say they take it on their profiles. Visit suburbs, small towns, and countrysides and see on the apps a few on PrEP there too -- and the numbers are increasing everywhere.
Jason Orne, a sociologist at Drexel University, has identified two narratives from his current fieldwork with gay, bisexual, queer or same-gender-loving people who take PrEP in Philadelphia. "When we're talking about this 'sexual revolution' narrative, I think it's important to acknowledge that, sure, it may lead people to not use condoms -- but also, great! This should be what we want, to help people experience sex without the fear of HIV."
After decades of emphasis in public health campaigns, "I don't think at this point additional pressure around using condoms is going to solve the HIV crisis, let alone solve anything involving STIs. I think we need new solutions, and I think we need to embrace people having the sexual agency for themselves to choose risk management strategies," says Orne. "I would argue that they're enabled to see sex as something primarily about pleasure and connection, rather than something one does when you get so horny that you're willing to overcome your anxiety and fear."
Some of those he interviewed reported that PrEP made them comfortable having anal sex more regularly or identifying as a bottom rather than as versatile or a top.
Orne's other narrative emerged from interviews with low-income, primarily black Philadelphians segregated from the gayborhood and "mainstream" gay culture. It reflects messaging from the free clinics and medical studies through which they, lacking health insurance, obtain PrEP.
"They see PrEP as 'Great, now I'm taking this. Now I am going to be a 'respectable' person who is monogamous, who only has sex in relationships, who uses condoms and uses them every time,'" says Orne. "It's not necessarily that these men are doing anything wrong -- from a public health standpoint, this is what people want them to do -- but I find it troubling when PrEP is used to encourage people to engage in more heteronormative behaviors."
"Queer communities have a unique and radical way of looking at sexuality as being part of a community, as about pleasure and as about autonomy and agency. I see PrEP as a technology and tool that lets people make those choices for themselves, and it bothers me when I see PrEP only viewed through a medical or public health lens alone," he concluded.
Quantitative studies have indeed identified a sizable shift away from regular condom use and a rise in STI diagnoses among people who take PrEP. A European man living in New York City said he didn't start PrEP to stop using condoms: "I started because I didn't want to be afraid of having sex. Not all of my sexual encounters included anal intercourse, but I wasn't feeling stressed and nervous when I was having it." He corrected my inference that he stopped using condoms because sex felt better without them: "Condoms are something that you have to stop sex to put on, something that you have to have with you -- and you don't have them all the time. It didn't have to do with pleasure: it had more to do with convenience."
Some men who are not taking Truvada for PrEP also report a change in the condom usage. One man in San Francisco let his prescription lapse "out of laziness" when he changed changed jobs and insurance. He is not rushing to get back on it, even as he rarely uses condoms during casual sex, because many of his sexual partners take PrEP: "S.F. is so super open about status that I feel I'm not at risk of contracting HIV. That said, regardless of whether or not I'm on PrEP, I always make it a point to ask about status for peace of mind." The "undetectable means untransmittable" messaging also has bearing on his behavior, and he has taken PEP in the past during scares.
A man living in a Midwestern city, undetectable for four years, said that he has seen more condomless sex in the age of PrEP. "As someone who enjoys bareback sex, I think it's been great," though some would-be bareback hookups who take Truvada still back out upon learning his status.
Another HIV-positive man in south Florida also said he has seen a turn away from condoms and credits PrEP with creating a more knowledgeable community. "I think more people understand what undetectable means and what true transmission rates are for HIV-positive men on antiretrovirals. People know what 'viral load' means, and I think PrEP served as catalyst for the conversation."
This has caused no small amount of soul-searching within the queer community. Michael Weinstein of the AIDS Healthcare Foundation notoriously called PrEP a "party drug" and has for years fought vitriolically against it as a public health tool. The "Truvada whore" slur was swiftly reclaimed and printed on T-shirts. California State University, San Marcos, communications professor Andrew Spieldenner writes of how PrEP usage can effect a "dirty/clean" binary. PrEP users can be slut-shamed as the former, yes, but they can also mediate a desire for bareback sex, overcoming its profound taboo in some gay circles since the AIDS crisis.
Columnist Dan Savage saw the first shift away from condom usage at the introduction of effective HIV treatments in the 1990s. "Along came protease inhibitors and the cocktail and the Lazarus effect and people stopped dying and the first issue of the Bay Area Reporter in forever came out with no obituaries -- it changed the calculus around people's risk-taking"
His first contact with PrEP came as an "extreme example" at the International Mr. Leather competition in Chicago soon after its introduction. "Someone hit on me and said, 'I have X number of loads in me already, and I would be honored if yours was next.' I was like, 'What are you talking about?' He said, 'Oh, no, it's OK. I'm on PrEP.'" He began to get calls and letters from people who had started using PrEP and stopped using condoms.
Savage believes all sexually active gay men should think about getting on PrEP but emphasizes that those who take it and make a decision to not use condoms keep in mind other sexually transmitted infections. He is wary of the expectation he sees in white gay urban circles that there is no need for condoms since all negative people are on PrEP and all positive people are undetectable, because he fears a return to the epidemiological circumstances that existed before AIDS. Aside from existing STIs, "Those of us who are old enough to remember before AIDS and after AIDS know that hitherto unknown sexually transmitted infections can emerge and kill everybody you know."
"We can't be pollyannas about this," he said.
"If we lived in a sane country that provided health care for all, we could end the HIV/AIDS epidemic in a decade or two," if everybody was tested and given PrEP or HIV treatment, depending on their status, says Savage. "Until we have a healthcare system that provides healthcare for all in this country, regardless of class, race, income, whatever, we're never going to be able to get to zero infections, because HIV seeks out vulnerable communities."
Even as PrEP is the closest humanity has yet come to a practical HIV vaccine, it is not widely taken. A 2016 demographic study estimated 4,503,080 American men have sex with men, and the CDC estimated in 2010 that well over 500,0000 MSM are HIV-positive. Last year, Gilead estimated that 136,000 Americans were taking Truvada for PrEP.
While the nationwide number of prescriptions for PrEP are rising, Gilead reports that those taking it are disproportionately white and over 90 percent are over the age of 25. Twelve percent of PrEP users are Latino and 10 percent are black; 24 percent of newly HIV-infected people are Latino and 44 percent are black. In 2015, the CDC reported that 22 percent of new infections occur in youth aged 13 to 24. While the FDA approved PrEP for adolescents last year, Teen Vogue has written that stigma and parental consent laws have limited its use among young people.
In 2014, New York state launched a campaign to limit new HIV infections to 750 by 2020. The number of recorded HIV diagnoses declined from 6,613 in 2001 to 3,702 in 2012, when the FDA approved Truvada for PrEP, to 2,881 in 2016. Among MSM New Yorkers, 1,580 tested positive in 2016, down from 1,804 the previous year. While the CDC's latest HIV Surveillance Report shows no change in HIV diagnoses among MSM has occurred since PrEP was introduced -- 26,052 Americans acquired HIV through male-to-male sexual contact in 2011 and 26,570 did so in 2016 -- Sherer points to declines in transmission rates in cities like Chicago and Seattle with robust PrEP advocacy campaigns to suggest the use of PrEP can turn the trend.
Truvada is extremely expensive: A month's supply costs well over $1,000, and there are substantial costs associated with the four-times-yearly clinical check-ins and screenings. Gilead's Advancing Access Program provides co-pay assistance for patients with insurance, though it is unavailable for those enrolled in government prescription drug programs like Medicare Part D, and a program also exists for patients without insurance who meet certain eligibility guidelines. The Patient Advocate Foundation's Co-Pay Relief program offers additional assistance to eligible applicants. Massachusetts has launched and California is launching a state drug assistance program. Some patients have taken to ordering generic forms of Truvada, approved by the FDA last year, over the internet.
Nevertheless, there are simply still uninsured people in the United States who lack the wherewithal or eligibility to acquire PrEP and insured people for whom the costs associated with PrEP are too high to afford, even with assistance programs. A 2016 report in Rolling Stonecites the malicious effect various states' refusal to expand Medicaid under the Affordable Care Act has had on impoverished people's access to medical care like PrEP, which Medicaid covers. It additionally pointed to limited transportation options to PrEP providers in low-income and rural communities, health care providers being unable to offer sliding-scale services to low-income people, and departments of health lacking funds to launch HIV-prevention efforts.
While a lack of access to PrEP, whether because it is financially impossible or because there are no nearby prescribers, is a demonstrated limitation to PrEP's spread, another limitation is the phenomenon of risk compensation. This is what Savage described: increased risk behavior spurred by a perceived decrease in susceptibility to HIV. Put another way, potential PrEP users do not get a prescription because they are apprehensive of potential judgment, and health care providers are wary of prescribing it for fear of giving license to riskier sexual behavior.
George Washington University psychologist Sarah Calabrese has written extensively on this issue. One study showed that surveyed medical students were more likely to presuppose a hypothetical black MSM patient would engage in barebacking compared to a hypothetical white MSM patient; study participants were less willing to prescribe the former PrEP. Another study showed limited racial bias from its sampled medical students, but those students "expressing greater heterosexism more strongly anticipated increased risk behavior and adherence problems, which were associated with lower prescribing intention." At any rate, most of the sampled students expected more risk compensation should MSM patients be prescribed PrEP.
Calabrese has led authorship of commentaries recommending specific actions and values for healthcare providers. She writes, "Penalizing the behavioral decisions of individual patients for the perceived good of the broader population is inconsistent with the professional obligation of providers to act in the best interest of their patients and violates expectations of patients when entering into a treatment relationship." Furthermore, she notes that many PrEP users were not consistently using condoms before getting a prescription and were therefore already prime candidates for PrEP.
In another study that speaks to potential patients' apprehensions about seeking PrEP, Calabrese recommends universally integrating discussion of the regimen into routine preventive health care for four reasons: to avoid missing potential PrEP candidates because of prescribers' biases, to destigmatize and normalize PrEP, to facilitate patient-centered care so that patients can decide whether PrEP is right for them, and to transmit knowledge about PrEP to the broader community through a patient's social network.
There is much more to be said about this phenomenon than can be expressed here with academic sources and cultural commentary. For that reason, The Advocate will publish reports on how Americans are interacting with this complicated miracle drug in different corners of these United States beginning in April:
In Portland, Ore., one of the queerest American cities, where we see a coordinated effort promoting PrEP by local government, healthcare providers and LGBT nonprofits.
In the Upper Valley region between Vermont and New Hampshire, a place with no gay bars, where a Dartmouth medical student is connecting rural New Englanders to PrEP prescribers over the web and through the apps.
In Albuquerque, N.M., a medium-size city with large Hispanic and Native American communities, where PrEP uptake is slow but advancing due to healthcare providers serving local communities.
In Northwest Indiana, which borders Chicago but lacks the Windy City's investments in PrEP access. We examine the repercussions of this disparity.
And in the heavily black Mississippi Delta, home to some of the highest rates of HIV in the United States, where we highlight the work of activists and nonprofits in overcoming barriers to care.
A slideshow of Americans from every state, the District of Columbia, and Puerto Rico reflecting on the effect PrEP has had on their lives will accompany the series.
AARON GETTINGER is a freelance reporter in Chicago. His website is ADGettinger.com.