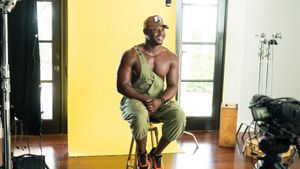
Devin Payne had gone years without health insurance -- having little need and not much money to pay for it.
Then Payne realized she's transgender. In her early 40s, she changed her name, began wearing long skirts, grew out her sandy blond hair and started taking hormones.
Although not all trans women get gender reassignment surgery, Payne said it was the right next step for her. For that, Payne, who is now 44, said she needed health coverage. "It is not a simple, easy, magical surgery," said Payne, a photographer who lives in Palm Springs. "Trying to do this without insurance is a big risk. Things can go wrong ... not having the money to pay for it would be awful."
Payne learned in the fall that she might qualify for subsidies through the state's new insurance marketplace, Covered California, because her income fell under the limit of $46,000 a year. She eagerly signed up in March for a Blue Shield plan for about $230 a month and began making preparations for the surgery that would change her life.
A "Preexisting Condition"
Among the less-talked-about implications of the Affordable Care Act is the relief it is providing to transgender people, many of whom are low-income and who have struggled to obtain health coverage.
Getting jobs that offer insurance often has been difficult for transgender people, and the cost of purchasing plans on the private market can be prohibitive. Some have been denied policies altogether after being diagnosed with "gender identity disorder," often considered a preexisting condition.
Without insurance, many people were unable to afford the hormones, surgeries, and counseling needed to complete their transition. Nor would they have been covered in the event of complications.
"We are still dependent on insurance and the medical community for us to be able to live authentically," said Aydin Kennedy, coordinator of the transgender health program at St. John's Well Child and Family Center in Los Angeles.
Now federal law prohibits health insurance companies from discriminating against transgender people, and it bars insurers from denying coverage based on preexisting conditions. That makes it possible for more transgender people to purchase private plans. And in states that have expanded their Medicaid programs, those with low incomes may get free coverage.
The federal antidiscrimination regulations have yet to be written, but California insurance regulators have said that companies must treat transgender patients the same as other patients. For example, if plans cover hormones for post-menopausal women, they must also cover them for transgender women. Medicare, the program for the elderly and disabled, lifted its ban on covering gender reassignment surgery earlier this year.
"The law and policy are on a transgender person's side for the first time," said Anand Kalra, program administrator at the Oakland-based Transgender Law Center.
A number of obstacles remain for transgender patients. Not many doctors specialize in transgender care. And while the law opens the door to insurance coverage, insurers can set conditions and don't automatically approve payment. "Insurance companies are making up their own rules as they go along," said Kalra.
And using government funds for these surgeries isn't without the usual right-wing opposition. "We would oppose sex change operations altogether," said Peter Sprigg of the Family Research Council, which is classified as an antigay "hate group" by the Southern Poverty Law Center. "But as a public policy issue, we would feel particularly strongly that taxpayers shouldn't be asked to pay for it."
"Feeling Complete"
Payne said her entire outlook on life changed when she started taking hormones.
"All my anxiety and all of the bad things that I felt inside were just completely washed away," she said.
Then when Payne was ready for the surgery, she started calling the approved providers in Blue Shield's preferred network. But they were booked up for months, or years. She felt she couldn't wait -- she wanted to do the surgery while her children were on summer vacation so they could go to her parents' house in Kansas as she recovered. So she found an out-of-network doctor in Palo Alto who would do the surgery.
"The time was right and I wanted to get it done," she said.
Her Blue Shield policy said that gender reassignment surgery could be covered if patients met certain guidelines. She had to be diagnosed with gender identity disorder, for example, and have an "expressed desire" to live as a member of the opposite gender from the one assigned at birth.
By the scheduled date, Blue Shield had authorized the operation but hadn't determined exactly how much it would pay for an out-of-network provider. Payne got a cashier's check for nearly all her savings, $27,000, to pay the doctor, hoping her insurance plan would reimburse most of it. She worried about all the other expenses too, including the hospital stay, lab work and anesthesiology services.
The day of the surgery at Sequoia Hospital in Redwood City, Payne said she remembers being wheeled into the operating room and feeling very calm. When she woke up, with oxygen still attached and wearing her hospital gown, a friend told her that the surgery had gone well, without any immediate complications.
Later that day, she had just enough energy to type a few words on her Facebook profile: "Feeling complete."
Grateful for Coverage
Payne eventually suffered a few complications -- some swelling and an infection -- but she recovered with medication and support from friends.
She is still trying to figure out how much she has to pay out of pocket for the surgery and hospital stay -- and how much of that her insurance plan will reimburse. Payne said she believes the lab work, pathology, anesthesiology services, and follow-up doctor's visits were all covered. But recently she got a statement saying she is on the hook for $17,000 of the total cost of surgery.
Payne said she will be grateful for whatever coverage she can receive. Her friend Jenny Taylor, who is staying with her during the recovery, has had an even harder time with her insurance.
Taylor purchased a policy through the insurance exchange in Tennessee. But she soon learned her doctor wasn't in the plan's network and that she had to pay cash for everything, with no hope of reimbursement.
"My insurance, even though I finally got it, was useless," she said.
The policy also won't pay for her hormones. A pharmacist told her the medication was for women, and her identification still listed her as a male. Taylor recently moved to Palm Springs and said she now plans to apply for insurance through Covered California.
"I was really frustrated," she said. "We're just trying to be ourselves, at the end of the day."
Listen to Payne's story in her own words in the video below:
This article was provided by Kaiser Health News, which is an editorially independent program of the Henry J. Kaiser Family Foundation, a nonprofit, nonpartisan health policy research and communications organization not affiliated with Kaiser Permanente.