The American Civil Liberties Union of Minnesota filed a lawsuit Thursday against the state's Department of Human Services, challenging the agency's ban on transition-related surgeries for low-income transgender people who receive Medicaid.
In OutFront Minnesota v. Johnson Piper, the ACLU is representing Evan Thomas, a transgender man on the state's version of Medicaid who was denied coverage for gender-affirming surgeries. Thomas is joined by OutFront Minnesota, the state's flagship LGBT rights organization. The state's public insurance program for low-to-no-income people is called MinnesotaCare.
Thomas has been diagnosed with gender dysphoria, and he currently receives MinnesotaCare, explained the ACLU in a statement. He has fought depression all of his life. This year his life was on an upswing as he forged ahead to be the man he always knew himself to be, beginning hormone therapy and legally changing his name.
As a low-income Minnesotan, Thomas takes advantage of the lifesaving health care available to him through MinnesotaCare. Although that program covered Thomas's medical need for hormone therapy, his public health coverage as a trans individual was limited: Vital gender-affirming surgeries were not covered in the insurance plan that nonetheless helps him with other health needs as a low-income person.
"A weight was lifted when I first began my gender transition and realized I didn't have to pretend to be a woman anymore," said Thomas in the ACLU's statement. But, he said, "being denied surgical treatment is harmful to my health and well-being every day I'm forced to live in this body."
Teresa Nelson, the legal director for the ACLU of Minnesota, tells The Advocate that the legal challenge is about "ensuring that transgender people are able to access the medical care they need to live a healthy and happy life." She says Minnesota's ban targets a group of people and denies them coverage "for no good medical reason," adding that such discrimination can be life-threatening:
"Minnesota's law and similar bans [can] only be attributed to hostility towards transgender people. The effects of this law on transgender people is devastating, not only because it denies them medically necessary care, but because it sends the message that the state does not care about their medical needs."
The World Professional Association for Transgender Health's standards of care for trans people stress that transition-related care is medically necessary, meriting health insurance coverage, and many advocates agree. The Diagnostic and Statistical Manual of Mental Disorders -- the American Psychiatric Association's guide for mental health classification and treatment -- defines gender dysphoria as a condition in which a person can experience acute distress, anxiety, depression, and even suicidal feelings because of a disconnect between their internal gender identity and the gender they were assigned at birth.
For many trans individuals, transition-related health care in the form of hormone therapy and various gender-affirming surgeries are powerful ameliorations of the suffering caused gender dysphoria, often allowing trans people to thrive as their true, most authentic selves. Gender-affirming surgeries may include body modifications like female facial feminization, male facial masculinization, upper body alterations, and lower body alterations for both trans men and trans women.
Ten states and the District of Columbia currently cover transition-related surgical care through their public health insurance programs. In the past year, states including New York, Washington, Oregon, Massachusetts, the District of Columbia, and Maryland updated their policies so that residents on Medicaid, a joint federal-state program, can obtain transition-related care. As expected, some conservative legislators and community leaders have pushed back on the trans-inclusive expansion of policy. When New York announced that Medicaid would cover transition-related care at this time last year, Rob Astorino, a Westchester County executive, decried the change as "ridiculous," joining State Sen. Martin Golden in criticizing what they felt would be the high costs of the coverage.
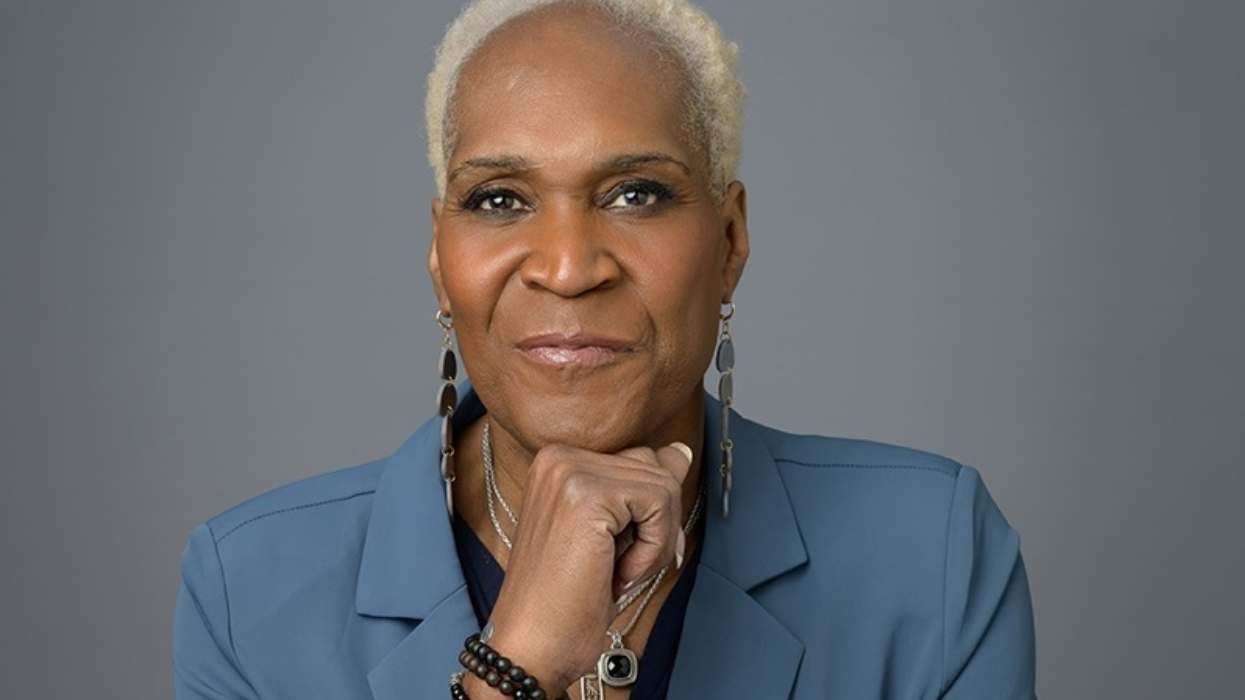
But advocates have long pointed to "the proven low cost of providing transgender-inclusive care, since transgender adults represent just 0.3 percent of the U.S. adult population." Illustrating the limited size of the population seeking such health care, a black trans woman named Kricket Nimmons this year became "one of the first low-income New Yorkers" to undergo gender-affirming surgery "paid for by Medicaid," according to The New York Times.





























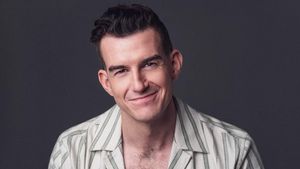





































Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes